| |
|
|
|
Posted ( jooosh) in All Posts on April-26-2010 |
|
|
to give a full update. Ella is stable…we’re exhausted…we will fill in the blanks later.
Thanks for understanding, and especially for the love and support.
G’Night.
|
|
|
|
| |
|
|
|
|
|
|
|

Thanks for all the support and prayers…and for understanding that we were too tired to post last night!
Ella has been stable. They finished weaning the nitric oxide at 12:15am last night. This is the biggest thing they like to eliminate before moving us from the PICU. This morning on rounds, they debated her femoral central line. It has been in her leg for 2.5 weeks, which is a long time and makes it high risk for infection. So far, so good. But there is an increased risk each day, so they’ve debated a PICC line in her arm. We spent most of the day yesterday without giving her food in her belly in preparation for a PICC line, only to learn that the PICC line nurses would not feel comfortable giving her a PICC line (too many scarred veins). In order to get one, they would need to send her to Radiology to have it completed. They would not give us a set time and Ella would need to refrain from any food or water via mouth or g-tube for 6 hours prior to getting the PICC line. We felt like spending all of today without giving food would simply set us back more (since we already did that yesterday).
During discussion today, the docs also feel like Ella has been doing so well that we are only a few days away from not needing the central line. Because we are only a few days away, they are willing to risk the infection with the central line. In that vein (pun intended), they have laid out a well thought out plan for switching meds to g-tube versus IV, weaning/switching diuretics, getting her to have more formula versus IV fluids, etc. Although the plan is thorough, we’ll need to see what Ella tolerates. It is great to think she will be at full feeds, for example, in three days. But history has shown that Ella can be slow with changes and moving too quickly might cause a problem. Then again, you never know! Ella is always keeping us on our toes.
Another concern: she’s been fluid positive for three days and her weight has gone from 14 kilos to 14.2 kilos to 14.6 kilos the past few days. These are usually her classic clinical signs to indicate fluid retention. So, we’ll want to watch her pulmonary status closely and look for any other clinical signs of fluid retention. For today, we have been safe to stay in the PICU but might be moved to the regular floor in the next 1-2 days, depending on how Ella tolerates all these changes.
She is doing well with feeds. Right now, we are giving a bolus of 80ccs every 4 hours. Her tummy seems to be emptying fine and she is tolerating all of it without much tummy discomfort too. To give you an idea, we need to get to around 230ccs every 4 hours to be on full feeds (6 feeds per day). So, I’m not sure if she will be able to jump from 80 – 230ccs per feed in just a few days, but maybe she will surprise us.
For diuretics, they are taking the Lasix from 20mg per kilo every 6 hours to Lasix 20mg per kilo once every 12 hours, plus Bumex 2x/day (1mg each) via her g-tube, plus Aldactazide via her g-tube. This is the same dose of Bumex that she had at 6 months old when she settled in Gainesville. The goal over the next 2 days: eliminate IV Lasix in an effort to pull the central line. We’ll see how that works.
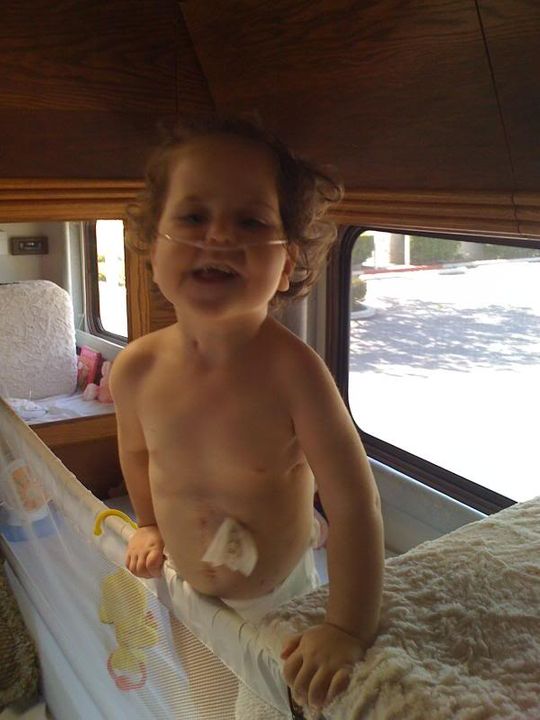
For withdrawal, they’ve decided to be more aggressive with weaning the Methadone and may wean the amount every other day while leaving Ativan the same. Once the Methadone is out of her system, they will get more aggressive with weaning the Ativan. It seems that we will likely be weaning the Ativan from home for a bit. Also in an effort to switch from IV to oral via the g-tube, they are going to start with Ativan tomorrow (any negative effects will show immediately versus Methadone can take 48 hours to show). Ella has still been having lost of withdrawal symptoms and waking up 2-3 times per night, requiring Atarax and Tylenol in addition to Methadone and Ativan to remain in a comfortable state and not too agitated. I think the picture shows how things get when she doesn’t get between doses of the withdrawal meds.

Ella’s thighs are bruised from having shots of Lovenox, twice per day. Since she is getting more food, they decided to switch her back to Aspirin and Plavix today. No more daily shots! These are her regular home medicines to help her superior vena cava stents from occluding.

Her new incision is healing nicely. The tape that was covering it finally came off on its own. I didn’t realize that they had to cut around her belly button!

Hopefully, all meds will be switched from IV to g-tube by Thursday. Then, we just have to wait for the feeds to increase enough to remove the TPN and lipids (IV nourishment). From there, they will look to remove the central line.
The other bummer about no central line: her labs. Right now, they are giving so much diuretic to keep her dry that they also are having to give up to three K-riders per day (potassium supplement via the IV) to keep her levels good. Without the central line, we will be back to sticking her again for labs which is always a challenge. Sigh…
If everything goes as planned, it looks like we might be at CHOC through the end of the week. But if Ella doesn’t respond favorably to any of the changes described, we may need to look to get a PICC line to keep IV access, minimize infection risk and give her more time to recuperate.
So along with general prayers for Ella’s health, please pray that she will not get an infection via her central line, which is close to her heart. These types of infections can be devastating.
Psalm 112:7 (NLT)
They do not fear bad news;
they confidently trust the Lord to care for them.
|
|
|
|
| |
|
|
|
|
|
|
|

It was a rough night again. Ella woke up five times, retching and crying in discomfort. Each time, it was near a dose of withdrawal med or in-between withdrawal doses, so we need to give Tylenol to help calm her down. The main symptom now: the ongoing withdrawal symptoms. She is touchy, gets agitated easily, and acts like she is on major drugs. It’s hard to experience her this way since her baseline behavior is so different. Normally, she is so happy. She is just cranky and agitated most of the day which is tough on the emotions hour after hour.
Ella had a repeat echo this morning. We haven’t received the official report, but just based on the preliminary report, it looks like the sildenafil is working and there is less cardiac and pulmonary pressure than any of the prior echos that she has had completed here at CHOC. She is on a double dose of Sildenafil, but at least we know it is working and being absorbed through her gut.
We decided to increase feeds today from 80ccs per hour to 120ccs per hour for three feeds and this evening at 8pm, we gave 160ccs. She is tolerating it well and is emptying better than we’ve seen even prior to surgery. They want to see her go at this rate for a couple more feeds and then increase to 200ccs per bolus feed. Our goal is 275ccs per feed. From what we can tell, it seems like she might make her goal fairly quick. Since she started doing well with feeds today, they turned off her TPN and lipids (IV nourishment).
We opted to decrease her dose of Miralax to one dose per day. She is stooling, but it is watery. Maybe she doesn’t need Miralax anymore since she does not have a bowel obstruction? It’s hard to know, but we’re hoping to figure it out in the next few days.
From a diuretic perspective, they gave the last dose of IV Lasix today and are just planning on giving Bumex and Aldactazide tomorrow. It would be ideal to wean the Bumex more in the next few days too, but that will not be a mandatory requirement for going home. We may just have to monitor this with her pulmonologist remotely from home for a handful of weeks.
For withdrawal, they weaned the Methadone dose today via IV and switched the Ativan to an oral dose via her g-tube. Since Ella did not seem to be doing well with her withdrawal symptoms, they increased the Ativan to 2.0mg per dose (versus 1.2mg), but instead of giving it every 4 hours, we are giving it every 8 hours. Tomorrow, they plan to wean the Methadone more and switch it to her g-tube versus IV. I think by tomorrow we might have everything (meds and feeds) switched over to her g-tube to where we can remove the central line tomorrow or Friday.
We tried taking Ella for a wagon ride today, complete with all of her attachments. Unfortunately, she was agitated the whole time. Normally, she loves that type of ride. Once again, I can’t wait to have my girl back.
Right now, it appears that we might be here for another 3-5 days. It will be so nice to be out of the hospital. I just wish she was sleeping sound at night. Currently, that impacts just my sleep but in the RV it prevents everyone from resting. So, we’re praying for a miracle recovery from withdrawal symptoms so that Ella can start feeling good again and all of us can sleep well.
We praise Him for our baby girl. We thank Him for her progress today with feeds and ask that He heal her body along with her withdrawal symptoms.
Psalm 29:11 (NLT)
The Lord gives his people strength.
The Lord blesses them with peace.
|
|
|
|
| |
|
|
|
|
|
|
|

Yep, we’ve been here three weeks today.
Ella only woke up twice last night. Both times, just like the night before, she would wake up retching. One episode last night stood out: she was up between 4:30am – 6am. At 4am, she was fed and then woke up at 4:30am with abdominal cramps. She was crying and I could tell her tummy didn’t feel well. We gave some Maalox to neutralize any acids in her tummy. Then, she had diarrhea real bad at 5am. This was the 3rd loose stool in 24 hours – it was watery. Then from 5am – 6am, she pretty much retched non-stop. If I didn’t know better, it would seem like she had the flu (vomiting and diarrhea).
During rounds, we discussed several steps. For pain management, take the Methadone from IV to g-tube. The pain management team came up with a weaning schedule that we will need to follow for Ella. Can you believe that it will take 2 MONTHS to wean her from Methadone and Ativan? I am still in shock. Once again, this is all because they have a standard care of protocol to not wean from narcotics when extubating, if it has been less than 5 days. Ella was intubated for 4 days and so they just cut off all the narcotics and she hit hard. This has been the toughest part of the whole experience. One thing is for sure: we know how sensitive Ella is to narcotics and will not go through this withdrawal stuff again without putting up a fight!
For diuretics, I was able to convince the docs to discontinue the loop diuretics (IV Lasix plus Bumex). Yesterday, we had 20mg per kilo of IV Lasix once and Bumex (1mg) twice, plus the Aldactazide. Right now, Ella seems really dry (she normally won’t drink water by mouth and she is begging for it). The IV nourishment always tends to make her more wet, but with the transition to formula, she probably does not need that much diuretic. Plus, they have been giving like 3 potassium supplements each day to keep up with what the diuretic is taking from her. Stopping the loop diuretics will definitely help with keeping her electrolytes in balance. It is a huge step, but we think she is now ready to go back to her Aldactazide, like she was on before this hospital visit. The oxygen was weaned this morning too – she is back at .5 liters and seemed to do well today. Once again, an indication of being dry.
One concern this morning during rounds: her white blood cell count was elevated from the past several days. It had been around 13 and it was 21 this morning. This was alarming only because they want to make sure that the central line does not cause infection. They took one set of labs in the afternoon to check potassium (it was 3.2) and plan for another complete blood panel in the morning at 4am. Then once Ella wakes up in the morning, they are removing the central line. This means that any other labs that are necessary will require a stick.
Another change: discontinue Miralax. It has been over 24 hours and she still has watery stool. Like I mentioned in the previous post, maybe she doesn’t need Miralax? Unfortunately even though we discontinued Miralax, we still were getting lots and lots of runny stool today. I’ve lost count on how many times she has been changed throughout the day. It’s a bit concerning too since she is retching so much more. So the night nurse thought about doing a stool sample, but each time she tried the stool was so watery that the diaper absorbed it. Getting a stool sample is the only way to determine if she has a parasite or not. We’ll see if she wakes up or has diarrhea throughout the night.
We are getting the indication from the night crew that it might be our last night in the PICU. So, we are weighing options and trying to figure out if Ella is ready to be discharged. Since we are pretty involved, it just might be worth taking the risk to deal with all the rest of her stuff from the RV versus moving to a different floor in the hospital for a few more days. But then again, I’d really like a few more days to make sure that this diarrhea is not something more serious and/or from food intolerance, that she stays dry enough on her diuretics, etc. We’ve made a lot of really aggressive changes over the past few days and I’d like to feel a bit more confident that Ella will not slip backwards before leaving the hospital. We’ll see what the docs tell us in the morning along with how her labs look, if she continues to have retching and diarrhea tonight and see how she behaves clinically.
Thanks for all the support and prayers.
Psalm 46:10 (NLT)
Be still and know that I am God!

|
|
|
|
| |
|
|
|
|
|
|
|
Last Thursday evening Ella had very watery stools for about three hours after her 8pm feed. We decided to hold off on giving any more food and with that she slept through the entire night. That was the first time she slept solid since we introduced food again. After some brainstorming and looking through previous blog entries, we came to the conclusion that the issue was mostly likely caused by too much food volume too fast. The docs tried to get her to take full feeds (250ccs) within a few days. It was just too quick, so the idea was to start over with smaller amounts and see if we saw the same reaction from Ella’s gut.
Yesterday morning Ella still had her central line in. We had thought that if she could move away from needing any IV access that we could just pull it and be done. But, with all the loose stools, unbalanced electrolytes, and not knowing the exact cause, we opted to get a PICC line placed. The fact that Ella hadn’t had anything to eat since 8pm the prior night meant she could go right to radiology have the line put in. But, the team that placed the PICC line was backlogged, it was on a Friday, and PICC lines aren’t done over the weekend! Well, nice that the Chief Medical Director happened to be in the PICU that morning. He was able to get us slipped in front of the queue!
With the successful placement of the PICC line, they were able to remove her central line later in the afternoon. After this line was pulled, we felt a little more relaxed with letting Ella be a crazy monkey in her bed. She just keeps spinning around, sitting up, tangling all her wires, which requires me to keep reminding myself that it’s a privilege to keep untangling them. =)
We started her food back up as well yesterday at 80ccs. Then bumped to 120ccs, then 160ccs. Unfortunately, she still had a very loose stool that evening and even another time in the middle of the night. This time, we’ve considered discontinuing her dose of Reglan, thinking that it may be contributing to the loose stools. So today is the first day without the Reglan. We had a feed at 8am (120ccs) and 12pm (160ccs) and so far, no diarrhea. If we could manage to discontinue Reglan, that would be great. The strange thing too: when we discontinued Reglan last May, we did have a couple of months where Ella seemed fine without it. But then we were hospitalized for a night due to feeding intolerance and the small bowel series indicated that she was not having gastric emptying, we started using Reglan again. Maybe that is when the bowel obstruction was starting and so she needed Reglan to help push things through? And maybe that is why she has required Miralax the past couple of months since we were hospitalized in Denver for a partial bowel obstruction? It was just the medicine she needed to move her system along. But now that she has had surgery, it would be great if we didn’t need to use either one of these medicines.
Ella’s lab numbers have all stabilized out, and she hasn’t really been that agitated either. The only side effects we are still experiencing relates to the Ativan which is keeping her in a perpetual drunken state. It can be funny to see sometimes but very nerve racking when she’s zooming around the crib and looks to do a face plant into the metal rails…oye. For this reason, we have to be vigilant in being right next to her when she’s active.
At this point, we don’t even have to work up to full feeds (1,375ccs per day). Even if we can get enough food and water into Ella to keep her minimally hydrated and nourished (1,000ccs), and her body can process it properly, we can look to head out of the hospital and work up on the remainder of the feeds on our own. Please pray she tolerates our feeding plan for the next couple days with no diarrhea!
Thank you again and again for all of you who have come by to visit, bring meals and/or have sent your support with cards and gift baskets. It has been one of the greatest gifts to us this time: feeling like there has been so much support in-person during our stay along with our virtual support on the blog.


When coming through all that we have, I find myself being reminded about the privilege that started over three years ago…
Being told by doctors in your home state of Colorado that your kiddo has a 20% chance of survival, BUT finding a surgeon in Florida who has a passion for saving these kids: a privilege.
Temporarily uprooting your life, moving to Florida, expecting to stay three months, staying eleven, multiple surgeries later, many heart wrenching days, lots of love shown by nurses, connecting with other amazing CDH families and friends, our precious daughter saved: a privilege.
Moving back to Colorado, watching your child grow, get strong, go through therapy, finding an amazing pulmonologist and pediatrician, going back into the hospital for reherniation surgery, connecting with more nurses and families: a privilege.
Still more therapy, multiple setbacks relating to food, drama with a nanny, the loss of a son, the doctor and many people who helped us get through it: a privilege.
Ella in the heart cath lab, SVC opened up, connecting with more doctors and nurses, Ella getting stronger, sitting, standing, babbling, crawling for the first time, back to the hospital in Denver for a partial bowel obstruction: a privilege.
Being able to travel with Ella in an RV all the way to California, seeing friends and family on the way, being close to CHOC when your kiddo has a major bowel obstruction, emergency surgery, four days of intubation, massive withdrawl symptoms, staying in the PICU for over three weeks, connecting with a single mom taking care of her precious son in the PICU, untangling all of Ella’s wires over and over again because she’s feeling better and acting more like herself, having a CHOC nurse be bold in asking to pray with us this morning: a privilege.
When we were in Florida, and Dr. Kays was talking about the plan for Ella and the potential future events, he raised the possibility of a reherniation. What was profound is what he called it if he would ever have to operate again: a privilege.
You see, having a kiddo that has been through all Ella has, all the complications, all the challenges, all the exhaustion, all the anxiety, all the tender sweet moments, experiencing Ella’s strength, her personality, her cuteness…all of this: a privilege.
Being able to share her story and have so many lives impacted for the Kingdom: a privilege.
Heavenly Father: Thank you for the privilege of being Ella’s parents. While it has to be the most challeinging and difficult thing we’ve ever experienced in our lives, the reward and privilege of having her with us is greater than words can truly express. Praise you Jesus for bringing her through the last few weeks, and all the many weeks before. Thank you Lord for letting us have her in this lifetime. Thank you for her amazing life. Thank you for her testimony of your Grace, Love, Mercy and Strength! May she continue to be a blessing to you as she has been to so many others. Amen

|
|
|
|
| |
|
|
|
|
|
|
|

The PICU staff was great to let us stay last weekend to see if we could get Ella ready enough to just leave directly from the PICU, but she wasn’t ready.
By Sunday morning, she was still having diarrhea and her potassium was not stabilized. During rounds, they looked at us and expressed that it was time to move. We really needed a GI expert at this stage since Ella was dealing with chronic feeding issues.


So, we spent Sunday getting ready to move – that sounds silly – but when you live in a room for 3+ weeks, you have to get ready to move! We had one of our favorite nurses for our last day in the PICU and then Ella’s uncle and a couple of cousins came by to bring lunch and give their well wishes.


Knowing that the transfer to the floor was pretty certain, we’d been expressing our concerns to the PICU staff and the nursing staff especially about going to the floor for infectious reasons. We try so hard to keep Ella from getting sick that we did not want to move to the floor, one step closer to leaving CHOC, and have her catch something. Most of the rooms on the floor are shared. Between the other patient plus any visitors they might have come to the room, it is a much less controlled environment to ensure Ella’s health stays intact. Along with health concerns, the chances of sleep are so much less with 2+ patients being attended to in a room. The rooms come with a chair to sleep in. It reminds me of when we were placed on the floor in Gainesville at Shands, only a couple of days after Ella left the NICU. Basically, a nightmare! Plus, there is no internet so it makes it hard to do blog updates.
Fortunately, our nurse asked for a private room for us earlier in the day and we were assigned a shared room. Before we were getting ready to leave the PICU, she called down again to ask if there was any way to get a private room. It worked – we got a small, private room. That was a major blessing.

We knew that going from the PICU to the floor was going to be an adjustment. We’ve done this several times. But we also have more than one hospital to compare. The first shift upon transfer, I felt like I was teaching the nurse how to do things. That is always an awkward feeling as a parent and not something that instills confidence. The hospital offers a chair to sleep in or a cot. I tried to get a cot – they were all taken. So the chair was my bed the first night. There was a bout of diarrhea along with an unsuccessful attempt for a blood draw, both which required assistance from the nurse. Plus, the construction of the new hospital is right outside the window starting at about 6:30am. Needless to say, I did not really sleep at all.

My lovely mother-in-law brought me a blow-up mattress yesterday so I could get some rest last night and it worked like a charm. Wow, sleep is a beautiful thing to get when you are running so low.
Yesterday, I wished I had more sleep to prepare me for the day. Nurses come by once every 4 hours to check. They really only came in the room because they needed to bring food and meds to Ella. I expressed concern at 6am to the night nurse about Ella’s PICC line not drawing for her labs. I brought it up each time to the nurse on the day shift – I felt like she was blowing me off. So when the charge nurse stopped by to check and see how everything was going, I vented my displeasure at the nursing staff and the docs on this floor.
She took it upon herself to help me solve some of my concerns, but to give you an example, it was 8pm before they resolved Ella’s PICC line challenge. It wasn’t drawing blood, so you order TPA, let it sit for 30 minutes to an hour, then it will break up the clots so you can get your labs. They had 2 other nurses come and try to draw the blood before they would order the TPA. It took from 6am – 8pm to get that accomplished with lots of nagging. I think the charge nurse recognized that she was the fourth person I had told and it was not right that I have to babysit that much for something that is relatively straight-forward. So, she also sent in the manager of the floor as well as the director of the floor to talk with me.
Along with the nursing staff, I did not care for the docs on rounds. I expressed concerns to them and did not see them the remainder of the day. Communication was not great in the PICU because the staff changed daily. It is not great down here because no one comes to talk to you. I expected someone, even a resident to re-visit once during the day to follow-up with the discussion from rounds and let me know the plan for the day.
Another example, a lady just walked in with a machine yesterday and said she needed a follow-up echo. The echo is no big deal, but couldn’t my nurse have told me that there was one ordered? Again, we have not had a great experience down here on the floor.
One welcomed doctor that came by yesterday: the GI doc. He was very nice and took in all the info on Ella. Then, he wanted to make some changes: change her food to Peptamin Jr. (it is partially broken down and has medium-chain triglycerides which have always helped Ella in the past). The current food she is on does not have the medium-chain triglycerides, so it just may not be optimal for her. Plus, he mentioned that anytime you have surgery and mess around with anything involving the guts, you almost have to start over. The things that may have worked before may not work any longer.
Along with changing food, he added back some vitamins with iron (similar to Polyvisol with Iron). We discontinued taking that when she turned 2 years old, but apparently it may help with food absorption. Also, he added Lactinex (Lactinex is a brand name for a probitoic supplement used to replace microorganisms in the intestines and colon, regularly found in unpasteurized milk products. It can be used to treat diarrhea resulting from infection or when an antibiotic regimen destroys the harmful bacteria).
It is Tuesday morning and since we have implemented the changes from the GI doctor, we have had no diarrhea. As a matter of fact, we have not had any poop. I take that as a positive sign that there is not something more major going on with her gut, like mal-absorption. Ella also slept great overnight. All of these are positive signs.
So what is going on today? I think all my advocating yesterday has turned into a better morning. I’m getting much better communication.
We’re going to try and remove the g-tube that was placed by surgery and put her g-button back in (surgery replaced her button with a long tube prior to surgery to vent the bile out moer effectively). With Ella becoming so much more active, a long tube hanging from her gut is getting in the way. The med port came open once and we fed the bed the other day. We just need it gone!
I’ve asked about accelerating the food since Ella seems to have tolerated her bolus of 160ccs so well. Switching to the Peptamin Jr seems to not made a bit of difference to her during feeds. And so far, it is even better because we do not have diarrhea. We’ll see what the GI doc orders for feeds the remainder of the day.
When they drew Ella’s labs last night, her potassium got stable at 4.1, which is right in the middle whereas just the other day in the PICU it was down to 2.6. Maybe without the diarrhea, it is leveling out. I discussed no more daily lab draws unless necessary. Down on the floor when they draw a lab, they take out 5ccs of blood as discard and then draw the labs they need. They do not put the discard blood back into Ella. In the PICU, they would put the 5ccs back into Ella to minimize her blood loss. After fighting that battle yesterday, the director on the floor was straight with me: the nurses on this floor are not trained to follow that protocol. So with Ella’s hematocrit (red blood cells that carry oxygen) being low, I’ve fought to limit the blood draws. The doctor this morning agreed with me and just stated that they would want one more before we leave the building. That works for me!
Ella seems to be stable on ½ liter of oxygen, her baseline at sea level. However, she has passed out 2-3 times since Sunday. That is way too frequent for me. In looking at her labs, her BUN is 4. On rounds, I asked for them to give me her ins/outs for the past few days to see if she is positive. Usually passing out too often can be Ella’s red flag for too much fluid retention. We’ll see how that turns out today too.
By the way we haven’t mentioned it recently, but Lola was feeling much better and has been able to return to “school” with her friends to play. Josh even found a local dog park to take her to over the weekend to run around with some other local dogs. Plus overall, she has been a great pooch, behaving and being obedient to commands. She’s been a great sport with this extended RV trip at only 10 months old. This has been a good, long extended intro to going on motorhome trips. I’m sure it will be old hat next time!


If Ella cooperates with the increases in food and we continue to have no diarrhea and her labs look good, I think we might be out of here by the end of the week.
UPDATE by Tina @ 12:15pm:
So they came in with a dose of IV Lasix. When I asked, she had been positive for the past three days by 1.2 liters. Within 30 minutes of giving the Lasix, she had a 200+ diaper. This explains the passing out moments the past few days. It also might mean that we are not out of the woods with having to give a loop diuretic to maintain her pulmonary status.
It’s been 24 hours since her last bout of diarrhea. We’re hoping to see some solid poop later or we will have to give a suppository!

Psalm 111:2 (NLT)
How amazing are the deeds of the Lord!
All who delight in him should ponder them.
|
|
|
|
| |
|
|
|
|
|
|
|

One step forward: we moved to full feeds as of Monday at 4pm and Ella seems to be tolerating the volume fine. We are giving 250ccs of Peptamen Jr along with 25ccs of water. She had the 4pm, 8pm and midnight feed on that schedule Monday and Wednesday was the first full day that we mimicked a true home routine. We’re excited that she is not having a problem accepting the larger bolus feeds. And so far, it appears that she is gastric emptying without any Reglan. Again, time will tell but we will be elated if we can discontinue that medicine.
Ella has been getting lots and lots of beauty sleep. I think the Methadone and Ativan are keeping her sleepy. Plus with full feeds in her belly, it tends to make her sleepy. I think the extra sleep is helping her heal and making her awake times more fun. She is crazy with exploring the hospital crib. She’s even sporting some new bruises on her legs in the exact spot that a 2 year old should have them!
With Ella’s new food, it was Wednesday, two full days later and still no poop. The GI doc was not real concerned, so we were not concerned. But we did agree: if she had not pooped by her 4pm feed, we would go ahead and give a ½ dose of Miralax to help things along. About 45 minutes after the 4pm feed and the Miralax, Ella pooped and it was not watery. That was nice to see. The docs confirmed that the Miralax had not been given a chance to take effect, so it was likely just Ella pooping on her own.
As of Wednesday, it seemed Ella was not saturating quite as well. When I asked about ins/outs, she was now 2 liters positive for the last few days. So the doctors decided to give her Bumex twice per day. We’re so bummed that we are back using such a strong loop diuretic, but all of her indicators show that she is too wet, including a weight from 14.2 to 14.9 kilos.
On Thursday morning during rounds, the doc was hopeful that we would maybe be discharged tomorrow. Since Ella responded favorably to the Bumex – he just wanted to see her labs to determine if her potassium was stable. Along with regular labs, we were also supposed to get a platelet blood study (recommended by the Hematology Department) to analyze how well her platelets are behaving with her current regiment of Plavix and Aspirin. This is not mandatory but they have a special blood lab at CHOC that can do this type of study, so we figured it would be interesting to take back to Denver.
When the nurse went to get the labs, she got enough to test the potassium and other electrolytes. It came back at 2.5 which is low. This was not a good sign, so they went ahead and doubled her g-tube dose throughout the remainder of the day, plus gave one extra dose right away to help counteract the imbalance. But when the nurse realized she did not draw enough blood for the platelet study, she came back to draw more blood and she could not get Ella’s PICC line to respond. This is the second time it has not responded since Sunday. So tomorrow morning, they are going to TPA the line before drawing another set of labs to check Ella’s potassium levels plus run the platelet study.
The withdrawal symptoms are still there – mostly she just acts like she has had a few beers. We get smiles and lots of normal Ella behaviors too. We’ve also been giving Atarax about once per day to combat the itchy symptoms. Otherwise, we thought the weaning plan was good because it is a tolerable amount of agitation and discomfort whereas early on, the weaning schedule was more aggressive and Ella was not responding well.

Two steps back: As of rounds Thursday morning, Ella was still asleep and seemed to be doing well. Once change for today: the Methadone was weaned from 1.5ml three times per day to 1.4ml three times per day. This is such a slight amount, yet it seemed like it was having an impact. When Ella woke up at 10am: retching and waves of nausea. Then, later she spiked a slight fever. You could tell that she did not feel well. It cumulated with diarrhea this afternoon – 4 rounds of it. When we spoke to the pain management team in the afternoon, they confirmed that her symptoms could be tied to withdrawal.
The more frustrating part: when the pain management team began asking questions, it was discovered that the nursing staff was not being consistent with the way that they administer the meds plus the times that the meds were being administered. Both are really critical with a narcotic weaning program, especially since Ella is so sensitive and not handling withdrawal the best. Because of the inaccuracies, they decided to revert to implementing the weaning plan from 6 days ago. In other words, they wanted us to start our 2 month weaning plan all over. All of this because of the lack of continuity in practice from the nursing staff. Even the time in the computer for administering the medicine had changed from the time that the docs wrote for originally. The staff did not have a good answer for why things were not handled correctly. So, they figured that if they go back 6 days and give Ella more Methadone and Ativan and the symptoms go away tomorrow, it likely confirms that it was withdrawal and it may mean that she is not ready for weaning and we need to go slower.
Tonight, we needed to increase her oxygen to 750ccs (a slight increase) to keep her saturating comfortably, especially while she was awake. We still think that even with using the Bumex, she might have more fluid she’s holding onto.
Things are not looking favorable for going home on Friday, as originally discussed. At this point, they now need to wait and make sure that the diarrhea is not food related, make sure the withdrawal plan is followed closely by nursing staff and that Ella is ready for weaning, that her potassium supplement is enough to keep her electrolytes in balance and that her pulmonary status doesn’t go south with all the extra fluid on board. As always, it’s really up to Ella.
It has been 4 weeks today and we are so ready to leave the hospital. Please continue to pray for Ella, wisdom for the doctors, and endurance for me & Josh.
Psalm 119:144 (NLT)
Your laws are always right;
help me to understand them so I may live.

|
|
|
|
| |
|
|
|
|
|
|
|

Ella had a rough couple of days.
She’s been stable on 750ccs of oxygen. We’ve had to increase it a little bit when she is awake, but the difference has been slight. Clinically, she seems nice and dried out.
The withdrawal symptoms have been tough. We’ve been weaning as outlined in the schedule laid out by pain management but we’ve had lots of retching, bad gas and diarrhea. Finally later today, we had one stool that seemed normal, but still lots of retching and gas. It seemed like it went from about 10am -4pm and stopped once she was finished stooling. The GI doctor does not seem overly concerned about the loose stools. He told us that if he gave one of us Peptamen Jr unflavored and asked us drink 4 cans per day, we might have loose stools too! He thinks that it just may take longer for her intestines to get back to normal. Plus, it could be some of these withdrawal medicines that are playing a role too. When her intestines settle down, we’ll also likely be able to return to the Nutren Jr with Fiber. Until then, the loose stools and foul smell may just be a reality for a while. The GI doc is willing to sign off and let us manage her at home as long as her potassium and chloride remain stable.
Her potassium and chloride levels have been all over the place. This is the last thing keeping us in the hospital. When they went to draw labs on Friday, the PICC line occluded. They TPA’d (tissue plasminogen activator) in the morning for an hour and still could not get it to draw. They TPA’d it again later for two hours and only one of the lumens finally drew. Her potassium was low at 2.6. So, they weaned the Bumex to 1x/day (the diuretic makes it tougher to keep her potassium stable), reduced her overall fluid input to 1200ccs per day (from 1375ccs) and doubled her potassium supplement. One other thing from the labs drawn on Friday: the hematology platelet study. They reviewed the results and the plavix and aspirin are doing the job of keeping her blood from clotting. This likely means that we should not see issues with her SVC again.
They needed another set of labs to check the potassium this morning. When they went to flush the PICC line this morning, neither lumen was drawing and it was infiltrating. This made a mess and got blood everywhere!


After they tried TPA again this afternoon for 2 hours and it still did not draw, they removed the PICC line. Later, they had to stick her to get labs. The only silver lining: God made it less painful as they drew on the first try which rarely happens plus her potassium was 3.4, which is much better. They want to draw two sets of labs in a row that show stable potassium levels. Literally, that is the only thing keeping us here.
The next set of labs is at 6am. I’m not looking forward to waking up that early myself much less wake up Ella to get labs, especially on Mother’s Day. Please pray that the blood draw will be successful without too much poking on the Bun. And please pray that her potassium is stable for the morning labs. If that happens, we might get discharged tomorrow. If not, then we will be forced to continue our hospital stay until they can get 2 labs in a row that look good.

As if it is not tough enough, we need more prayers for Lola. As of yesterday morning, she got sick again too: vomiting and diarrhea. Last night, she woke Josh up every 2 hours needing to go to the bathroom. This means we can’t take her to the doggie daycare nor leave her unattended for much time and not expect an accident. So far, she’s been really good. Today, Josh gave some Kaopectate (peppermint flavored) and some Pedialyte. For dinner, white rice and boiled chicken for the pooch. We’re hoping she gets better real soon.
A Mother’s Love
by Helen Steiner Rice
A Mother’s love is something
that no on can explain,
It is made of deep devotion
and of sacrifice and pain,
It is endless and unselfish
and enduring come what may
For nothing can destroy it
or take that love away . . .
It is patient and forgiving
when all others are forsaking,
And it never fails or falters
even though the heart is breaking . . .
It believes beyond believing
when the world around condemns,
And it glows with all the beauty
of the rarest, brightest gems . . .
It is far beyond defining,
it defies all explanation,
And it still remains a secret
like the mysteries of creation . . .
A many splendoured miracle
man cannot understand
And another wondrous evidence
of God’s tender guiding hand.

|
|
|
|
| |
|
|
|
|
|
|
|

Wow, it has been a crazy couple of days.
Ella’s labs looked satisfactory on Sunday morning, with her potassium at 3.9 (ideally between 4.0 and 4.5). Armed with that knowledge, we fought to get discharged. The prior couple of days had been so frustrating with the nursing staff. Things like waiting an hour for a dose of Tylenol, feeding Ella 1.5 hours late, etc. We would try to give input based on knowing Ella and we had to fight for everything – they were not giving us any credit for knowing her. At that point, we knew we could manage her better outside the hospital and did not need to stay any longer. We even promised to come back for labs to be drawn outpatient to check her electrolytes. The bottom line: we were just done with the hospital.

It was Mother’s Day, so what a nice gift. We left the hospital around 11:50am and then I had to hurry and get ready back in the RV because my aunt treated me to a girls afternoon complete with a massage. Then later, a dinner that included prime rib. Yum! But normally this could not happen with our current situation in the RV (one person can’t take care of Ella and the dog, a sick dog nonetheless). So, my uncle offered to babysit Lola. What a great Mother’s Day gift. It gave me about 4-5 hours of disconnecting with the realities of life.
Fortunately while I was at the Mother’s Day festivities, Ella seemed to be stable while Josh was overseeing her and getting used to her new schedule. She has so many new medicines, new food, etc. She seemed still a little buzzed from the meds, but definitely acting more like herself and exploring her space in the RV.

But by the time I came home and as the evening progressed, Ella did not seem to be doing well. When we put her to sleep and put the pulse oximeter on, she was only saturating in the mid 80s. Not good. We turned up the oxygen to 1 liter. Still not much better. We turned up the oxygen to 2 liters. This put her in the mid-90s. What the heck? We checked all the lines, the tank, her cannulas, changed the pulse oximeter, etc. It all pointed to the fact that Ella probably was fluid overloaded. Even though it was late, we gave her a dose of Bumex and planned to follow it with a dose of potassium in the early morning.
Throughout the night, she was restless. With her withdrawal symptoms, she is not sleeping well. Josh and I were both up several times to console her and changed diapers twice. This was good – the Bumex was working. I could tell she was better after the first diaper and we turned down the oxygen to 1 liter. We left her there the remainder of the night. The good news at this point: Lola seemed to be a bit better because she was not asking to go to the bathroom all night.

From the first feed at 8am on Monday morning, Ella became fussy. She was retching a lot throughout the entire day, especially the morning into the early afternoon. It’s not even related to feeding her. You can vent and try and draw back. Sometimes you get air, but very little food. And it doesn’t stop the retching. This is what we have seen though in the hospital these past couple of weeks: she just has nausea and it is likely due to withdrawal. Today the Ativan was weaned slightly, likely part of the cause. Also, she did not poop yesterday when we brought her home from the hospital. Today, we decided to wait before giving Miralax. We did not want any diarrhea!
In the early afternoon, Ella seemed like she wanted to go to the bathroom. Then, she broke down and cried. It smelled like there was poop. Sure enough, Ella experienced her first constipation. Wow, one extreme to the other. There was a brick of poop in her diaper. Larger than a golf ball, smaller than a racquetball. I still can’t believe that came out of her! This was the cue to give a dose of Miralax. We’re going to try 1/2 capful each day of Miralax going forward and see if that helps her out. It’s always a trial and error, but we’ll figure out just the right amount in the coming days.

In the meantime, Josh and I were both fervently working to get Ella everything she needs. I was having to make calls to ensure that food was being delivered to us. We only have enough until Tuesday morning. That took several calls. We needed new prescriptions. We called a few places, but most needed too much time to turn around. With hesitation since we were not happy with CHOC, we contacted the outpatient pharmacy at CHOC, assuming that they have everything we need. Without going into all the details, Josh went back and forth to the pharmacy four times. We were even charged for things in the end that we should not have been charged for. Then, our pharmaceutical insurance was giving grief over Ella’s sildenafil prescription. They wanted us to pay $2,491 for a 30-day supply! We still have to iron that out tomorrow morning plus the pharmacy still owes us more of some of the meds. All in all, that was a nightmare that required elevating the situation to the Director of the Pharmacy. Yikes!
I did call and speak to Ella’s pulmonologist in Denver to give him and update and asked for some input on giving Ella more diuretics, enough potassium and checking labs later in the week. He was very helpful. After talking, we decided to give an increase in Ella’s aldactazide diuretic (6ml, twice per day) and one Bumex each day, followed with one dose of potassium supplement. If we think she still needs to be dried out, we can give another Bumex and potassium supplement. Whatever we feel like works, follow the plan for at least 2 days and then go and get labs checked. It’s so nice to have someone helpful yet someone that also trusts us to manage and care for Ella. He knows that we are Ellaologists!
Then, I had to call the hospital back and page the resident that worked with discharging us. I had to ask for a standing order for labs, so we can check as we need. There was some challenge because they want us to follow-up with a pediatrician. I explained that we are following up with one, but just not here in CA. We want to work with her primary caregivers from CO but get labs here locally. Finally I was able to convince them to fax the labs to our pediatrician and write the standing order. Yikes…once again, not real impressed with the standard of care from the regular floor at CHOC.
Tonight, things got a bit better. Ella’s numbers looked so much better than last night. She is on her baseline of 1/2 liter of oxygen and saturating 98 right now. Way different. Also after two doses of Kaopectate and rice with boiled chicken, Lola had her first solid poop in three days. So tonight, both girls are doing better.
Work, what’s that? Please pray that Josh and I can continue to fight the battles we need to get Ella her medicine and food in the next 24 hours. And somehow, that we will find the time to bill some hours for work. Also, that Ella will remain stable, be dried out enough, handle the weaning of the withdrawal meds and have good stools! Finally, that we have figured out the right Ella cocktail for now which will mean good labs in a couple of days and that we can enjoy our last week or so with family and friends outside the hospital.
Thanks again for all the support and prayers. It’s only been about 36 hours since we left the hospital and I’m still processing that we just spent 1+ months at CHOC on our CA trip in our motorhome…and right now, we are spending the last few nights sleeping in the motorhome in a church parking lot. It’s been a crazy journey and we’re so thankful for all the support from all of you out there.
1 Corinthians 16:13-14 (NLT)
Be on guard. Stand firm in the faith. Be courageous. Be strong. 14 And do everything with love.
|
|
|
|
| |
|
|
|
|
|
|
|

The last couple of days have not slowed down.
We thought Lola was getting better, but as it turns out, she is still sick. Josh was up several times last night taking her out to go to the bathroom. She is still eating and drinking water, acting like herself. But her poops are still way too runny. You can’t even pick them up. We’re trying to monitor closely and taking turns walking her. In the meantime, it requires two people to care for her and Ella. It’s not like we’re at home and can just open a sliding glass door to the yard and tell Lola to go outside and take care of things on her own. Maybe Lola just has sympathy pains for Ella?

On that note, Ella’s had runny stools the past 2 days. We’re still dealing with the art of how much Miralax to give her. After trial and error, we’re going to try 1/4 capful per day starting tomorrow and see how it goes. When we gave no Miralax, she was constipated and would not stool for days. When we gave 1/2 capful over the past few days, she’s had runny stools. Now, we’re going to try in the middle to see how that works.

We took a picture of just Ella’s first round of morning meds at 9am. These don’t even include 2 that she gets at 6am or the long list of meds the rest of the day. Can you believe this is just one round of meds for the day? We turned one of our gift baskets into a med basket; this doesn’t even show the meds that are in the refrigerator. Wow, crazy how medicated our child has become these days.

We’ve had so many nightmares in dealing with CHOC the past couple of days. We’ve run into all kinds of problems with the pharmacy – they’ve overcharged us for items, inadvertently charged our credit card twice, etc. One example: there was a 30 day prescription that costs $40. Then, there was a charge for $14 for the same medicine. When we asked, they explained that the $14 charge was for the portion of that med that was given to us at discharge. First, the cost of $14 for 2 days worth of meds doesn’t calculate right if a 30 day supply is $40. Second, I have never had that happen. When you get discharged and they give you enough for a 24 hour period, it is part of the hospital bill that they charge the insurance company as part of the hospital stay. Last, we asked what happens if we went to another pharmacy to get these prescriptions refilled. They admitted that they would need to write off the cost and not collect the money. So, we’ve already spent ~$200 on prescriptions and will spent hundreds more when sildenafil gets resolved in a couple of days, and yet if we would have gone to Walgreens, for example, they would not have been able to collect that extra money. So we are getting punished for giving them our business? Plus, they did not disclose that they were charging us for the meds on discharge date. We only found this out when we examined the receipt and called back, escalating it to the Director of the Pharmacy. This is only one example of the types of things that we’ve encountered.
The saga continues as we are trying to still get Ella’s sildenafil (Viagra) prescription refilled. We’ve contacted Josh’s prior employer for their help with the pharmacy insurance coverage. They agree that although this medicine is not normally covered, they’ve given exceptions the past 2 years for Ella since it is medically necessary. It’s been 2 days and we are still waiting for the red tape to get settled between the company and the pharmacy insurance provider. In the meantime, we only have a few days left of this particular med so I’ve been calling a few times a day to see if we can get it resolved. One thing is for sure: this medication is medically necessary and we cannot pay $2,500 just for a 30 day supply of one med! Hopefully once we get the insurance side of things worked out, the CHOC pharmacy will cooperate and submit it with the correct drug code so it will go through properly.
Another nightmare: it turns out that CHOC will not call in an order for us to get labs. They know it is vital that we check Ella’s potassium and chloride levels along with her other electrolytes since she is on Bumex and potassium chloride supplements. It turns out that it is their way of ensuring that we go to a pediatrician within a couple of days to get a prescription for a blood draw. Um, we expressed that we do not have a pediatrician locally and that we will not be home for a couple of weeks. Plus, that we want to work with Ella’s normal care providers to review results, but the Denver doctors cannot call in an order to the CHOC outpatient lab because they do not have rights to practice at CHOC. I have tried to get this resolved since we left the hospital on Sunday. We even asked the nurse as we were leaving and we were told that we did not need an order – we could just walk in and tell the front desk that it was for a follow-up to an in-patient stay and they would do it. Wrong! Once again, we liked many on the PICU staff but the regular floor staff along with the pharmacy is not real good. It just confirmed how blessed we are with Ella’s team of healthcare providers in Denver along with the hospital. Maybe that is one of the reasons we need to stay in the Mile High City for now.
We spoke with Ella’s pulmonologist on Monday and finally reached her pediatrician today (he was traveling). We caught up on all the details including the debacle with the labs. He can call and order labs at an independent blood lab called Laboratory Clinics of America. They have locations nationwide. This will work and we are going to go get labs tomorrow. This is ultimately the right solution and what we wanted – but – I’m still floored that CHOC would not give us an order for labs. We’re hoping that her labs come back stable because then we can just continue to do what we have been doing the past 3 days. It means that we can go until we get home without sticking her again. If the labs don’t look great tomorrow, we’ll need to talk to her primary providers, make changes/adjustments to meds, wait a couple of days, then go back for more labs.
As if we don’t have enough things to worry about, Ella woke up this morning and she is sick. We thought we heard some coughing and some signs yesterday but it came to full fruition today. She has a cold with a real bad cough. Right now, she is still saturating ok on 1/2 liter of oxygen, but we pray that it does not go into her lungs. That would be really bad and require hospitalization.

Along with her cough, we also noted a firm nodule under her skin on the left side of her neck (behind her ear near her hairline). When I spoke with the pediatrician today, he reassured me that it is likely a lymph node that is inflammed due to her sickness. Apparently, it is common in young children. Ella’s had colds before, but never gotten a jelly belly size nodule in her neck. This was just another thing that made our hearts sink. Can’t she get a break? So between yesterday and today, Ella has not been up crawling around like you noted on the last blog. We’ve had slight grade fevers on and off, coughing, retching, snotty nose, general fussiness. She just doesn’t feel good and is resting (or trying to) for most of the day.
We’d like to have stable labs plus make sure Ella’s cold is getting better and that she is going in the right direction before we head home. As it looks right now, we’d like to leave Tuesday or Wednesday next week to start the journey. It will still take 3-4 days to make it back to Colorado. We’re hoping that everything falls into place.
We did move from the church this afternoon. I still can’t believe the generosity of the Orange County First Assembly of God church – they let us park our motorhome at their facility for an entire month! That was truly an answer to prayer and we will be forever grateful for the generosity during such a time of need.
Isaiah 43:1-2,4 (English Standard Version)
“Fear not, for I have redeemed you;
I have called you by name, you are mine.
When you pass through the waters, I will be with you;
and through the rivers, they shall not overwhelm you;
when you walk through fire you shall not be burned,
and the flame shall not consume you.
…Because you are precious in my eyes,
and honored, and I love you”

|
|
|
|
|
|
