I will try my best to summarize the roller coaster recovery details. Warning: this is going to be a long post!
Once we went upstairs to the cardiac unit and were in a room on Wednesday night, there was about an hour till shift change. The initial nurse was great. However, shift change occurred and it was evident from the introduction that we might have a challenging nurse on our hands. The nurse had lots of experience and that part was appreciated, but she wasn’t as keen on taking input from parents. Being Ella-ologists, that always poses a problem for us since we are very involved.
We started feeding Ella at 8pm – she handled her bolus of food great. She did seem extra thirsty, so we were having to get up, prop her in the bed and give her juice frequently. Then at 10:30pm, we ran the food pump. It was about this time that Ella fell asleep. Unfortunately being at the hospital, the sleep is always interrupted. At 11pm, they used her IV to run a bunch of strong antibiotics in her system and followed it with a flush. At 12 midnight, they wanted vital signs so she was disturbed at that time too. Each time, it took some soothing to get her back to sleep.
While she was asleep, we were able to turn down her oxygen to 750ccs. This is what we have done at home before when she is doing really good, although admittedly, it has been a while since we have been able to do that at home.
We crashed about 12:30am. All three of us slept for about 2 hours. At 2:30am, Ella woke in writhing pain. She was screaming loud. It seemed to come on suddenly. The only medicine I had in the room that I could give was Tylenol, so I gave it to her via her g-tube.
We paged the nurse and started talking through what could be going on. She didn’t seem to sense the urgency that this was not normal. Then, Ella started having bouts of diarrhea. The nurse thought it was probably the antibiotics. We were convinced that she was having some GI/belly pain and needed something to treat it. We mentioned that we would like some Maalox (it contains agents to soothe her tummy along with Simethicone (aka Mylicon) to help if there is any gas). It worked like a charm when we were in-patient at the Children’s Hospital before with Ella.
The nurse informed us that they don’t give Maalox – ??? We knew that was not true. It became apparent that the cardiac unit does not give Maalox. This was a bit frustrating because we could tell that it would help Ella, but for some reason, the nurse did not want to get it for us. We asked to see the doctor. This is when we also learned that the cardiac unit does not have a doctor on the floor overnight. The only doctor available is based in the cardiac intensive care unit. So, they have to page the doctor and the doctor uses the nurse’s thoughts via phone to give orders. So, the nurse said that she would page the on call doctor to talk through it.
In the meantime, Ella was screaming and crying so loud every couple of minutes. The pain was coming in waves, which also told us it was GI/belly related pain. Our room was near the nurse’s station, so I asked Josh to leave the door slightly open, so the nurse could hear. Once she came back about 30 minutes later, the doctor decided to order Toradol, a nonsteroidal anti-inflammatory drug for management of moderately severe acute pain. It is like giving her a stronger dose of Tylenol via her IV. Once again, we were convinced that it was not that type of pain. We agreed to go ahead and give it to her, but once again asked for Maalox and were turned down. We told the nurse that if this does not alleviate in 15 minutes or so (since it was given via IV), that we were going to need another solution. The nurse thought it was maybe the food. So, we vented her and no gas was present. And just to eliminate it as a variable, I turned off the food pump.
The time passed and it was not getting better for Ella. Josh went out to see if we could get somewhere with anyone, since our nurse did not seem intent on helping us. And by this time, Josh was worked up and we were both venting a bit. It was 3:30am and Ella had been in pain for an hour. There was no doctor available and they would not give us Maalox. Our nurse was adding fuel to the fire rather than trying to calm him down and really help us. She could have tried to apologize and relate to our frustration. Instead, she just tried to defend the system. We’ve received better care at this same hospital, down the hall under the pulmonology team. When we were first admitted, we asked to be under the pulmonology team, and it was a big political thing. They said that the pulmonology nurses would not be comfortable dealing with whatever might surface in Ella since she had a heart procedure completed. Since we thought it would only be for one night, we conceded.
So, after arguing for another hour, we found another nurse that was willing to call and get the Maalox ordered for us. It arrived at our room at 4:30am. We gave it to Ella. It immediately coated her stomach and she fell asleep. She did not make another peep. It is exhausting to be an advocate for your child, especially in the middle of the night!
All three of us fell asleep until 7:30am, when the door opened and they wanted a chest xray. Ella was sleeping, so this was not going to be good. But it was one of the things we needed in order to see if we could go home. Shift change had already occurred, and from about 3:30am forward, we never saw our nurse. I needed to make sure that food was going to be on its way and see if we could get another order of Maalox on hand, since that clearly seemed to help Ella.
So, I woke Josh and asked if he could do the chest xray. In a daze, he sprung off the air mattress and started to help. He did not realize that Ella’s oxygen had been turned down to 750ccs. The xray tech was not the best and was taking his time which was making Ella even more upset. Ella desaturated very fast and required 2.5 liters to get her to recover from the ordeal. The color in her face was bluish-purple and she did not look good. It was a healthy scare. It took her about 20 minutes at the higher level of oxygen to come back to normal. Even then, her eyes were purple and she did not look good. Aside from the oxygen scare, I think it was simply because she was tired and needed more rest. Josh was convinced that something was not right with her. Either way, it was not a pleasant way for Josh to wake up and it got his anxiety started for the day.
The day nurse started off on the wrong foot with us. It seemed like the night nurse maybe tainted her view. For example, when she first started the shift I asked her to see if we could get more Maalox on hand in case Ella has more belly pain. She replied with, “Well, from what I understand you are going to be discharged and then you can give your daughter whatever medicine you want.” What kind of response was that? Fortunately, we approached her again when she returned to our room. Instead of being defensive, she apologized and handled it professionally – this turned the situation around. She was great the rest of the day and even complimented us on being great advocates for Ella.
The nurse gave more antibiotics, so I was expecting more discomfort for Ella. Sure enough, we changed the bed several times from diarrhea blowouts. Plus, for the rest of the morning, Ella did not look great. She also spiked a fever of 101.8. She was requiring 2 liters to 2.5 liters to maintain saturation in the mid-90s. A nurse practitioner visited our room and told us that Ella’s right lung showed effusion. This would explain the higher oxygen requirement. However, 30 minutes later she came back and stated that she was looking at another child’s xray.
In the late morning, Dr. Fagan and Dr. Abman’s nurse practitioner came by for a visit and noted the higher oxygen requirement. They thought she might have extra fluid on board from the procedure. It is common for them to administer IV Lasix to help many kids get off the extra fluid. Knowing Ella, this seemed logical. Since everything else was looking good, they gave Tylenol for the fever and wanted to watch her and go get more opinions on the Lasix idea. We told them that Lasix might be a good idea, but we would really like to get labs to see where she is at before giving it to her. At this point, it looked like we’d be staying another night. Since that seemed like the case, we started asking to be switched to the pulmonology service. We did not want to spend another night under the cardiology team.
The remainder of the morning, Ella slept for a few more hours. With the Tylenol, her fever reduced over time. The nurse assistant came to complete the EKG which was normal. Also, it seemed like slowly her oxygen requirement was coming down which was good to see. When I would wean the oxygen, she would do okay but if she got upset, you would have to turn it up right away. She was not able to rebound well. At this point, she was back down to her baseline requirement of 1 liter.
In the early afternoon, the tech came by to do the echocardiogram. She was very experienced and really nice. She understood that Ella was not likely going to like the echo and made sure to just get the pictures she needed. While it was going on, she was showing us the flow of blood in/out of her SVC and commented that there was “good flow”. Heck, it was apparent right on the screen. That was great to see. And although Ella did not like the echocardiogram and still complained, she was tolerating it better than the chest xray and EKG. This told us that she was beginning to feel better.

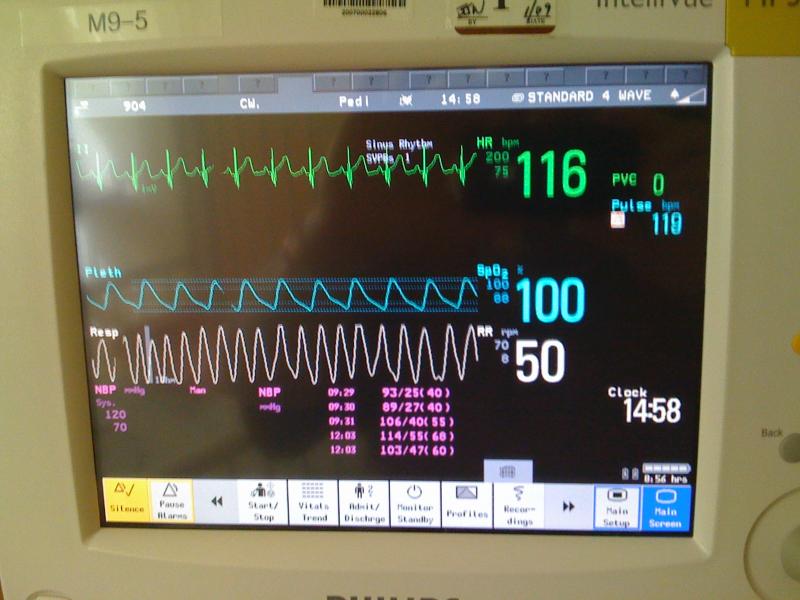
Ella decided to take another nap and Josh decided to go down the hall and escape in the view. It was about 2:45pm. This time when she went asleep, she was saturating 100 on 1 liter, so I decided to wean the oxygen. I turned it down to 750ccs and waited a few minutes. Her saturations were the same. So, I weaned to 500ccs and waited several minutes. Once again, saturations the same. I was in disbelief. I turned the dial down to 250ccs (1/4 of a liter) and waited. She settled in between 96-98 on saturations and a heart rate between 110-120. She was not ever on 250ccs even in Gainesville at sea level! WOW!
I sent a text to Josh’s phone and told him to come back. He replied, “Good or bad?” I replied, “Good”. He walked in and I pointed to the monitor. He seemed pleased, especially since she was not even looking that good this morning. Then I asked him to go look at the oxygen regulator on the wall. He was in disbelief. We sat there in amazement for several minutes. As a test, we turned off her oxygen to see what would happen. It took about 1 minute for her to go down into the high 80s. Normally, a few days ago, it would only take about 20 seconds to go into the high 70s. Once again, wow!
As we were sitting there enjoying this break, a voice came across the speaker system throughout the entire hospital, “Code Blue in the Cath Lab, Code Blue in the Cath Lab.” For those of you without as much hospital time, code blue meant that a kid was crashing/dying and they were asking for all resources available. Ella was just in the cath lab the day before. Emotions came over both of us and we began to feel sad for the family that was waiting and hearing that message over the speaker. We said a short prayer for that family and at the same time, thanked Him for bringing Ella through her procedure.
Once Ella woke from her nap, she was on 500ccs awake and 250ccs when asleep. The fever had gone away and it seemed like the further away we were from the last dose of antibiotics, the better her tummy was feeling. They came to draw labs; it was Susan, a resource nurse, that was familiar with Ella from our last stay. When she came in and noted the IV, she recommended that we try drawing off of that line. That has never worked for Ella, but we agreed to give it a try. It drew blood so we did not have to poke Ella again. Later, the labs came back looking good and in-line for Ella. Based on a good chest xray, EKG and echocardiogram, plus the fact that her oxygen requirement was lower, they decided to let us come home. Keep in mind too, we never gave her any additional diuretic. They talked about it, but then she improved on her own. We have not seen Ella improve like this before without additional diuretic!
It was about 6:15pm by the time we officially left the building. We were just so glad to not be there anymore! They asked us to watch her bowels and her fever. If either continued into today, her pulmonologist asked us to page him.
Ella still kept me up most of the night – she was up about 10 times. Between doing that Tuesday night, no sleep Wednesday night and very little last night, today consisted of sleeping for me! Fortunately, Ella did great today. She did not have a fever and her stools are returning to normal. She was in a happy mood while she played with Kelly.
We can already see that Ella’s body is responding well to this procedure. We’re so thankful for the miracle of getting her SVC open and hope and pray that lots of good breakthroughs can come from it – like being off of oxygen and medicines sooner. Only time will tell. We also pray that her body will accept the stents and that it will not try to re-occlude through the stents. We were told that is a possibility, so we need to have tests done every so often to check the flow in her SVC to make sure her body is not trying to re-occlude the openings.
Thanks again for all the support and prayers…and for rejoicing with us. We feel that this was the medical miracle that Ella needed to move forward and progress.
Colossians 3:15 (NLT)
And let the peace that comes from Christ rule in your hearts. For as members of one body you are called to live in peace. And always be thankful.


