Ella’s day was a bit more rough – yesterday was definitely the honeymoon to get us through the coming days and provide hope.
The docs wanted to make too many changes and Ella rebelled. First, the pain management team came up with a plan to wean the Ativan from 1.5mg to 1.2mg. After a couple of hours, she started to have withdrawal symptoms. She was more shaky and just seemed agitated. Fortunately, no itch but she was clearly uncomfortable in her own skin. We ended up giving the missing amount of Ativan plus a little extra just to settle her down. The plan was to wean Methadone tomorrow. At this point, I’m not sure if they will still try or not. Throughout the day, I did notice that if the nurse was not regimented about giving one of the withdrawal meds on time, Ella let us know.
Along with Ativan, they increased her food from 5ml to 10ml per hour. We tried giving 10ml over 30 minutes and venting/resting for 30 minutes on and off. A few times though, we got clear tummy pain. When we would vent, we would get return that was a bit green in color and TONS of air. Sometimes when venting we could connect her manually with the syringe and nothing seemed to happen. But if we drew back on the syringe, we got lots and lots of air. Also, we would get anywhere from 20-40ccs in the syringe. This meant that she was not emptying as quickly. This has been our concern all along: slow gastric emptying and slow motility. Since she seemed to be having tummy pain and we wanted to see if it was her tummy versus lower intestinal pain, we got approval for a dose of Maalox. Thankfully that did the trick by neutralizing the acids in her tummy and within 10 minutes, she was calm.

Later in the day, I convinced the nurse to give her a rest from the feeds. We drew back in the syringe and she had 40ccs of formula in her belly. When you’re only feeding at a rate of 10ccs per hour, it was clear that she was not emptying real well. However once we vented all the air out, we could bolus the 40ccs right back into her via gravity, and she tolerated it fine. So we decided to give her a 2 hour break and I convinced the nurse that this was an example of how Ella tolerates bolus feed schedules better. We waited 2 hours, gave 20ccs of formula and didn’t bother her again for 2 hours. The good news: I don’t think that the formula is giving her any problems or discomfort. Plus, she had another poop tonight. This means that overall things are working. We just need to be patient on moving forward with the volumes and make sure that the gastric emptying and motility is working.
Another symptom today: tons of mucoids. Wow. Just lots of really thick secretions. Since she was so thirsty, we were giving water by mouth which was helping to break them up. But then she would cough, retch and soil the bed. We had to change it a few times. Thankfully, Josh and I were both here when these happened and Josh was able to grab Ella and lean her over so the mucoid would come out of her mouth onto the bed instead of her re-swallowing them. Along with mucoids, she was retching a lot. Oh, I wish that retching was not a daily activity. Just as we’ve noted before, it is definitely associated with her feeding via g-tube. When we were not dealing with food the past 2 weeks, we had no retching. Somehow food must be refluxing or just the pressure of her belly having something in it, even just the smallest amount is causing the retching.
The docs decided that Ella was not outputting enough urine, so they’ve increased her Lasix to 20mg per kilo every 6 hours. Plus, they are still giving Bumex, here and there. She had one dose of Bumex this morning and a chest xray is scheduled for the morning to check her fluid status. Right now, she is even on ins/outs for the day. I know that this will be another area where we need to try and wean to get back to a reasonable dose of diuretics for our trip home. We are able to dry her out to this extreme in a hospital setting where they draw labs and check her electrolytes all the time. But once we are back to a home routine, we cannot give this amount of diuretic. I’m bummed that we’ve had to use Bumex this hospitalization (we went 14 months without using it at all). It will just be interesting to see how the diuretics end up working out this round.
Her central line has been in her femoral artery (her thigh) since her day of surgery, 2 weeks ago. There is a decent amount of risk for infection as the days continue. And we have several days of hospitalization ahead of us where we need to be able to give IV meds, IV drips and do blood draws. So the plan is to switch to a PICC line on Monday (peripherally inserted central catheter). A PICC is inserted in a peripheral vein and then advanced through increasingly larger veins, toward the heart until the tip rests in the distal superior vena cava or cavoatrial junction. The last time she had a PICC line was the NICU. Hopefully, they can get it on the first try.
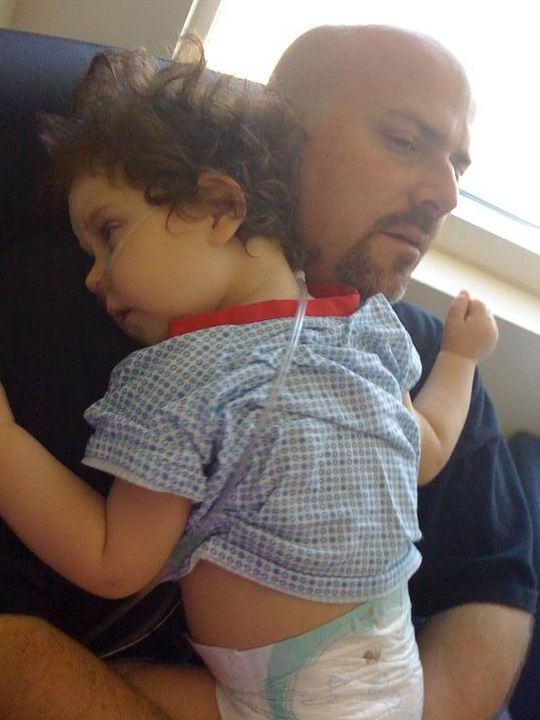
One cool thing: my brother and sister-in-law know a physical therapist that works here at CHOC. I ran into her today and asked for a favor. I wanted to see if we could get one of those chairs to sit in Ella’s crib. I figured it would help drain secretions and help with gastric emptying. Plus since Ella still acts like she has had a few beers, it would allow her to sit up and not work quite so hard. Apparently, the rehab/physical therapy department does not normally come and leave their tools in the PICU because they end up getting lost. But she made an exception for Ella due to the connection with my family! It will be a nice tool to use over the coming days.
In between the fussy times of discomfort and sedated moments from withdrawal meds, we did see glimpses of Ella. She would get excited, smile and play. Although the day was a bit rough, we still made a tiny amount of forward progress with feeds. We’ll see what tomorrow brings.

