| |
|
|
|
|
|
|
|
As a follow-up to yesterday (I was too tired to write), we went to Dr. Perry’s office for her 12 month well check. We had a great visit.
Ella weighed in at 15 lbs, 12 ounces and 27 1/4 inches long. She is getting bigger! We discussed the notes/strategy from the nutritionist that visited last week. Until the swallow study is complete, Dr. Perry increased her food intake 50 ccs total. So now she is taking 700ccs of formula each day. Her caloric intake is lower than it should be, so the increase in Alimentum should help. Once the swallow study is done and there are no concerns, we will reconvene and come up with a new feeding strategy. We’re hoping that we can resume with solid foods and phase out Alimentum to a pediatric formula, likely Peptamin Jr.
Retching has been a common occurrence with Ella these days. It used to occur in Gainesville, but seemed to be tied with feeding and volume. For some reason, it has increased since our return to Colorado (several times daily). But now, it is not related to feeding and she is retching HARD. It still seems to be directly related to secretions in her esophagus that she does not know how to manage (they block her airway). So, she coughs, then gags, then retches. Dr. Perry mentioned several ideas including dryness tickling her throat to maybe she is retching more because she is not eating orally and using the esophagus muscles. After discussing all the variables that could be impacting it, he wants her to go see a pediatric gastroenterologist to look at her esophagus and check out her nissen fundoplication. In addition, he increased her dosage of Reglan 50% from .4ccs three times per day to .8ccs three times per day.
A few days ago, I ceased giving her juice because she is retching so much that I am concerned about aspiration. Instead, I am simply giving her water. Dr. Perry expressed that water is good for her and to let her have as much as she wants. The good part is that it does not seem like we have to be as conservative with fluid restriction in her diet. Today, she drank 8 ounces of water – – that’s a lot for her.
Ella had some granulation tissue build-up on her g-tube, so Dr. Perry burned that off. Also, he provided us with some silver nitrate sticks so that we can manage that at home in-between appointments.
We discussed that we are anxious to try weaning the diuretics. We’ve always been concerned about the high dosage that she has been taking for so long. Dr. Perry recommended that we have labs taken in the morning before she sees the pulmonologist in late August, so we have a baseline. Plus, she hasn’t had blood labs done in a while and it is always good to check her electrolytes.

Ella also received her 12 month vaccinations. They did it just the right way – quick, fast. Two nurses came in and gave two shots in the each leg simultaneously and then two shots in each arm simultaneously. As you might expect, Ella did not like this part of the visit. But at least they understood to not take forever to administer 4 shots. I had to increase Ella’s oxygen and do lots of comforting afterwards, but she calmed down within 5 minutes. That’s pretty good for Ella – – earlier on this journey, she would not calm down that quickly when she would get upset.
It is so cute to see Ella interact with Dr. Perry. She likes him. She was rolling around on the table, kicking and grabbing the paper lining. Then, she would roll over and hand her binky to him or grab the hair on his arm! He mentioned that he can see a lot of forward development in Ella since the first time we visited. It is always good to hear that kind of perspective.
Ella, Grandma West and I hung out today at the house. Grandma West looked for projects to do – she found the swing that Grandpa bought for Ella’s birthday and put that together (Ella had a swing in Gainesville, but we sold it on Craigslist before coming back to Colorado). It will be good to put Ella in a swing again. I think we’ll try it tomorrow.
The Bun spent more time in her high chair today. The sessions throughout the day were for 5 -15 minutes, depending on her tolerance. I’m just placing her in it and distracting her the best I can to try and get her used to being in the chair. Eventually, if we get the “ok” to begin eating solid foods again, I’d like to have her eat in the chair! It would be a nice routine as we start that type of therapy again.
Aside from all this info, she had a great first birthday and is still the cutest Bun ever! By the way, is that a thumb I see?

|
|
|
|
| |
|
|
|
|
|
|
|

We are practicing sitting in the new high chair. Today was pretty good. We had 3 sessions lasting 15 minutes each. They may not sound like a lot, but that is great progress for Ella.
This afternoon Grandma West left to go back home. We are sure going to miss her!

|
|
|
|
| |
|
|
|
|
|
|
|



And yes, she even crosses her leg when she’s getting beauty sleep!

|
|
|
|
| |
|
|
|
Posted ( jooosh) in All Posts on August-2-2008 |
|
|

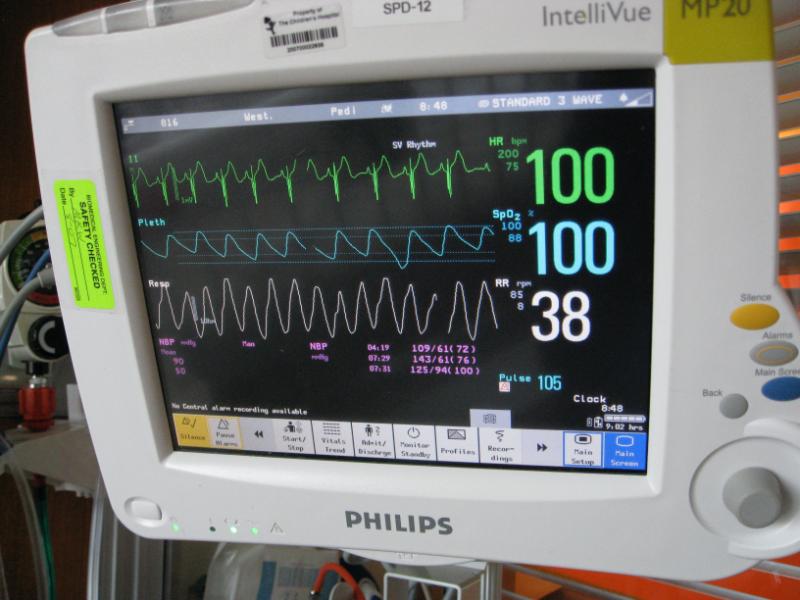
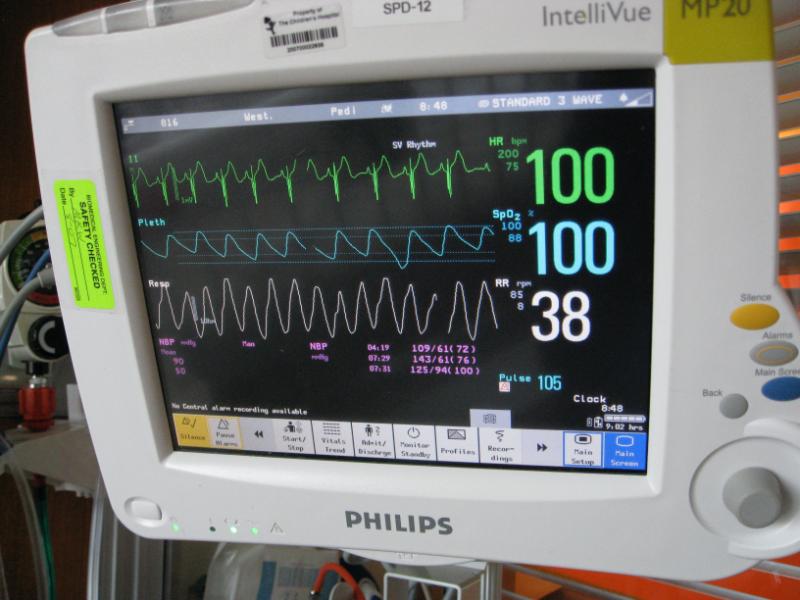
We had a bit of an early morning scare with Ella today. Something woke me up around 2:30am this morning, and I decided to go check on Ella. Her heart rate was fluctuating between 145 and 155 bpm and she wasn’t saturating that well (upper 80’s, low 90’s). She also felt a bit warm to me.
Normally I would go wake Tina up and get her thoughts, but because I tend to overreact in these kind of situations, I decided that it wasn’t critical enough to justify waking her up. I continued to check on Ella for about an hour, and then finally fell back to sleep.
Tina went in to check on her around 6:15am and I could hear Ella in the monitor. She began to cough, and then she began retching. It sounded like she couldn’t catch her breath, and then she started getting real upset. I went into the room to see if I could help Tina.
I immediately became alarmed because her heart rate was over 200bpm! We’ve seen her do this before while she was in the hospital, but not since we’ve been home. My anxiety was compounded by the lack of sleep so what started as good intentions to help Tina, turned into Tina having to take care of another upset individual.
Of course I was thinking worse case scenario at this point, even invisioning her just having a heart attack or something. I was also feeling guilty because maybe I should have done more earlier that morning.
Well, after Tina calmed Ella down a bit, and talked me out of rushing her to the Children’s Hospital, she reminded me of something I had thought of, but had since forgotten.
Ella did have her vaccinations about a week ago, and I thought this might play a part, but previously she would spike a temp within 48 hours or so. Tina then told me that the doc said we might see this happen in a week or two. Ahhhh….maybe that is what’s going on.
I went down to the kitchen to get some Tylenol for Ella. We gave her one dose then and another a few hours later. By noon her fever had broke.
We all got out of the house today and ran some errands around town and did some repairs on our rental properties.
So my scare this morning reminded me of last year when Ella was still very sick in the NICU. Man…talk about perspective. As you can see from the picture above, it’s still a very long way from where she used to be.
Praise God we have our little girl here to love. She is such a miracle.

|
|
|
|
| |
|
|
|
|
|
|
|

Ella has not been herself the past 24-48 hours. Along with the increased coughing and retching, you can just tell that she doesn’t feel that great. The smile above was one of the rare glimpses throughout the day.
She felt warm, so we gave her Tylenol a few times today. Dr. Perry told us to expect that Ella might have a fever for 24-48 hours due to the vaccines. If Ella doesn’t seem improved by the morning, we will be calling Dr. Perry. These symptoms started last Friday night, but seem to be sticking around.
Her retching was so bad this morning that she passed out briefly. She has done this a few times to me over the past few weeks. But Josh was taking care of Ella this morning when it happened. It freaked him out a bit. I don’t think he has ever seen Ella get that bad with retching.
It all seems related to secretions and congestion. And today both of those things are worse. Who knows, maybe she has a bit of a cold or something. She has been breathing through her mouth more, since her nose seems to be more congested, and she seems to be requiring more oxygen.
Even at night while asleep, she is requiring more oxygen and her heart rate continues to be higher than it should be – – higher than her baseline.
When you can’t get Ella to break much of a smile, even with coaxing and funny faces, you know that she isn’t feeling well. Typically, these symptoms do not point to a good direction for Ella.
Please pray that the Bun will begin to feel better.


|
|
|
|
| |
|
|
|
|
|
|
|

UPDATE – 8:00AM (MST) (by Josh):
Tina called Dr. Perry this morning (Ella’s pediatrician) because she had another rough night. Due to her continued fever, high heart rate, and overall behavior, he recommended that she take her to the ER to have her checked out. Hopefully some tests will give us more insight into what’s affecting our girl. It could be something as simple as a cold, or maybe something else. I’ll update once I know more.
While riding on light rail, listening to Charles Stanley this morning, God put this thought on my heart. Do the circumstances around us make God any less trustworthy? In ALL circumstances, we can fully trust in Him. Praise God!
UPDATE – 11:30AM (MST) (by Josh):
Tina just let me know that Ella’s being admitted to the hospital so they can watch her overnight. Not a ton of info yet, just doing all the tests…xray, echo, labs, etc in the ER before they move her to a room upstairs. One doctor said the chest x-ray looks hazy… and that maybe her lungs are wet, but they look ok otherwise…no collapsing or signs of aspiration. We’re waiting to see what Dr. Abman (her pulmonologist) thinks. White blood cell count looks ok, so it doesn’t look like infection. She’s also not running a fever right now. She’s currently on 700mls of O2 and saturating about 95%. Heart rate is around 150. We’ve also noticed that her urine output has decreased over the last day or so.
At this time we think it may just be the fluid issue Ella has always battled, but we’ll see.
Praying and trusting.
UPDATE – 11:00PM (MST) (by Tina):
Once all the tests were done this morning, we were stuck in the ER until 4:30pm. The Children’s Hospital had every bed filled to capacity, so we were waiting for someone to be discharged. They wanted to admit Ella to the hospital so that they could run more tests and monitor her overnight.
They moved us to the eighth floor. It is a private room complete with a flat screen TV, pull out bed, bathroom and view of the city and mountains. Along with the beautiful facility, all the employees have been amazing. We have never been to a Children’s Hospital and it makes such a HUGE difference when everyone is trained to take care of children. If we have to be in the hospital, we are glad to be here. It makes the experience not so bad.
This evening, Ella has stabilized on 1 liter of oxygen. Along with her fever that returned tonight, her heart rate is around 185, breaths per minute 85-100, and saturating 93-95. So far, all her tests are not pointing to anything obvious. Her white blood cell count was normal. Blood labs came back with everything in normal range, although her blood urea nitrogen (BUN) came back at 14. If you remember, a higher number means that she is more dry and Dr. Kays liked to see it 20 or higher. The last BUN was 18, when we first returned to Denver. So she is definitely more “wet”, even though she is still on a lot of diuretics.
They took a blood gas this evening and said that it was pretty good – – they expected it to be worse, but it seems her body is compensating. For all the medically minded people out there, here were the results:
PH – venous gas 7.45
PCO2 – Venous 47
PO2 – Venous 54
HCO3 – Venous 32
Total CO2 – Venous 33
Base Excess – Venous 7.0
O2 Saturation – Venous 87.3
The chest xray came back looking slightly hazy, but not real bad. It is tough for them to comment because they have no other chest xrays to compare. Her echocardiogram shows no pulmonary hypertension; this means her medicine is working and the altitude is not causing too much of an issue. The swab for viruses (they swipe boogies from her nose) came back negative. So far, no bacteria growth for the other blood tests.
Dr. Perry called and we discussed everything that happened today. He is such a great doctor – so nice. Tomorrow, Dr. Perry will be attending on rounds so we will get to see him in person. We are going to try and have some tests completed tomorrow through gastroenterology – – we want to figure out why she is retching so much and if that has played a role in her lungs getting too wet (could she be micro-aspirating)?
We expect to be here throughout tomorrow and possibly for another evening, depending on how Ella does throughout the night. Once we meet with all the doctors and they discuss the results of all the tests tomorrow morning, we will have a better idea.
Thanks for all the thoughts and prayers for the Bun. The support out there from all of you is so encouraging during times like these.

|
|
|
|
| |
|
|
|
|
|
|
|
Sorry for the delay in updating today. It was a packed day for me and the Bun.
Ella slept well last night and seemed to be stable, so the nurse reduced her oxygen to 750ccs. Once she woke up, I expressed to the nurse that it seemed like she needed more O2 while she was awake. So, the nurse put it back to 1 liter.
We went down to radiology at 10:15am. Too bad I did not have a camera of Ella riding in the Red Wagon down to her procedure. It was pretty cute. She sucked her binky and held onto her frog pillow while watching the ceiling tiles.
They used imaging liquid to check her nissen fundoplication. We wanted to make sure that the wrap was still intact. The good news: everything looked alright.
We are still scheduled for a swallow study this Thursday at 2pm. Unfortunately, I think we still might be in the hospital. So the silver lining is that we can conveniently just wheel on down to have our tests done. The swallow study should answer a lot of our questions that we have been having about Ella’s recent retching with secretions and oral food intake. Also, it should help us come up with a strategy for increasing her calories and a better idea of what we can feed her orally over the coming days.
Once we came back, I fed Ella – – she was tired and very hungry (she had not eaten since 6:30am; we needed an empty tummy to check out her nissen). Once I fed her, she took a nap. When she woke up, she seemed like she was laboring more in her breathing. I kept watching her numbers and behavior. She was still on 1 liter of oxygen, but pretty congested and breathing through her mouth more. The pulse oximeter showed her in the low to mid 90’s, but then dipping down into the low to mid 80’s and not recovering quick. The process of dipping down into the 80s was happening more and more.
I mentioned something to the nurse. She watched, but then Ella would creep up into the 90’s, so she didn’t feel any action was necessary. That was my double-check or second opinion for the time being.
Later around 4pm, Ella began to complain to me a lot. She was clearly having a tough time breathing. She was staying in the 80s more and more. She looked dusky and was breathing labored and fast, with a heart rate around 185. She needed more oxygen and she was letting me know clinically by her complaining too: she was grunting. The flow meter in the room only went to 1 liter. I couldn’t locate the nurse. So I walked to the other side of the bed and grabbed the blow-by oxygen. Ella seemed to respond favorably and crept up into the low 90s. This was my confirmation that she did indeed need more oxygen – it was not my imagination.
At that time, a case manager came in to talk with me. I expressed my concern with her and she indicated that she would go find my nurse for me. Without going into a lot of detail, Ella down spiraled in approximately a 15 minute time frame. She ended up on 2.5 liters of oxygen and required blow-by oxygen to stabilize.
During this episode, they decided to draw labs again and ordered another chest xray. I had not even seen the initial xray, so I asked the doc to take a peek. As soon as I saw it, my gut instinct kicked in and confirmed it: Ella is once again retaining fluid. Her BUN is 14 and she has too much fluid on board; she does so much better when she is more dry.
The biggest change since we came home to Denver is that we were told she could have diluted juice and/or water orally, so she has been having a lot more fluid input over the past weeks. Although it was slow, it might have made the difference. She has always been fluid restricted in the past. This is the only change I can think of related to fluid input.
After going back and forth with the various doctors and sharing her history (this is a teaching hospital too, so you have to explain things over and over to several people), they decided to give her more diuretic. I explained how IV lasik works well for Ella and that it might help get the fluid off her more quickly. Since they did not have an IV yet, they opted to start by giving her an extra dose of Bumex (she gets it 2x per day, so they added another dose). Also, the pulmonologist opted to give her a steroid for the next 5 days to help with lung inflammation called Prednisolone. Hopefully, this will just help her regain strength.
The biggest challenge now: we need peripheral access. They tried to get an IV yesterday with three different people, including a charge nurse. None were successful. Today, they sent someone with a “good stick” that was able to draw labs and did not see anywhere to get in a peripheral IV. So they called the charge nurse in the NICU to come and try. She tried three different places and was not successful.
At this point, they want IV access since Ella’s condition has gotten worse. They do not want to be in a place where they need to administer in a critical situation and not have access.
Our nurse thinks that the only people on shift tonight that might be able to get an IV is the flight team. So we are going to check with the flight team to see if they might be available to try. Honestly, I am not sure how/where they are going to try. She has been pricked several times in various locations. Literally, I don’t know how it will work – – maybe a miracle?
The only other option is a central line, but that is more invasive and Ella doesn’t have a great past with those either. When they did that in the past, her IVC partly occluded.
While I was typing this post, the flight team came into the room. They surveyed and the RN found one spot she thought might work. Josh went outside and prayed fervently. The whole process was about 40 minutes, but they got an IV in her left foot. Praise God – – that was a miracle. Now, Ella is sporting a sexy go-go boot and we are waiting to see if the night crew wants to give her a dose of IV lasix.
Thanks for all the outpouring of support and prayers for the three of us. Please say a special prayer for Josh. He is feeling very stressed, exhausted, and emotionally raw. He is just having a really hard time watching Ella endure this latest challenge.
Yes, this is another valley in the journey, but we know He is ever-present and with us each moment in the hospital, as He is every day. Our prayer request is for a smooth evening for Ella, that the diuretics will begin to do their magic and that her oxygen requirement can be weaned in the next 24 hours.
Psalm 121
1 I lift up my eyes to the hills—
where does my help come from?
2 My help comes from the LORD,
the Maker of heaven and earth.
3 He will not let your foot slip—
he who watches over you will not slumber;
4 indeed, he who watches over Israel
will neither slumber nor sleep.
5 The LORD watches over you—
the LORD is your shade at your right hand;
6 the sun will not harm you by day,
nor the moon by night.
7 The LORD will keep you from all harm—
he will watch over your life;
8 the LORD will watch over your coming and going
both now and forevermore.

|
|
|
|
| |
|
|
|
|
|
|
|
UPDATE – 1:20AM (MST): Ella is not sleeping well. She is going in and out of sleep with a bit of fogginess. She seems disoriented. This is new. I wonder if it is the steroid that she received at 6pm; she’s never had that drug before tonight (Prednisolone). The nurse stated that they give this med to asthma patients frequently and it can have a restless effect. I know that she is overtired, but something seems different. She was crying like she was in pain and would not take her binky. I hope she isn’t working too hard.
Also, they decided to give her IV lasix at 12:15am; she’s had one diaper weighing in at 115. Anything over 100 is a good output for her.
On a positive note, her heart rate is around 110-115 and she is saturating 100 when she is still and asleep. I have not seen her heartrate that low in several weeks. I just wish I was seeing those numbers while she was on her baseline amount of oxygen, but she is still at 2.5 liters. Please say a prayer that she will go to sleep and rest soundly! She is so tired…and Mommy is too!
UPDATE – 2:40AM (MST):Yep, we’re still up. Ella is continuing this strange behavior, on and off about once every 15-25 minutes. They tried giving Tylenol earlier at 1:20am, but it didn’t seem to do much. The doctor gave her another full examination and thinks that she looks fine. She simply attributes it to a combination of possibly the steroids, but mostly that she is sick, doesn’t feel well and maybe has an overall achy feeling. Please pray that Ella can sleep away her discomfort and that there is not something else going on!

UPDATE – 8:45AM (MST):Ella and I did not sleep well last night. I’m convinced that it is the steroids that kept her up and had her feeling jittery and uncomfortable (look at that hairdo!).
We were woken up at 6am because the night shift team wanted a blood gas and so they wanted to poke her again. Literally, she has been poked 10+ times in the last 48 hours. I guess her potassium was a bit low yesterday and then they gave her lasix, so they want to check the levels again. Since they have used all good veins, they ended up trying in her hand and resorting to a heel prick.
I’m pushing for a plan and strategy today from the day shift team. I don’t feel like we have one central point of contact. And at this time, I’m not clear on what their goals are for her over the coming days. Do they want a clear chest xray? Do they simply want her saturating well with a good heart rate at her baseline of oxygen requirement? Are they going to give her more diuretics? Are they going to want more blood gases? What are our goals for her? All of the above? As you can see, I’ve got lots of questions. I’m hoping the day shift team can help answer them today.
Although we had a rough night, she is looking a lot better this morning. She is down to 1.5 liters of oxygen. She doesn’t seem to be working as hard. Right now, she is watching a video in her crib – her heart rate is 128 and she is saturating at 97-98, with some feet kicking going on. Yesterday, her heart rate when she was awake was around 175 for most of the day.
She still sounds sick – congestion and coughing. But the fact that she is not working as hard makes me feel better.
I feel like the fluid issue is subtly being confirmed. They gave her an extra dose of Bumex yesterday as well as IV lasix. Her urine output on Monday was ~300ml. Her urine output yesterday with the increased diuretics was 535ml. So, she definitely is getting rid of some fluid (normal range for her would be 168 – 336; 1-2mls per kilo, per hour).
The fluid theory is also being confirmed when you look at her weight. She weighed in with the ER at 16 lbs 4 oz (7.47 kilos) and this morning she weighed 15 lbs 6 oz (7.1 kilos). That is a big weight shift between Monday morning and Wednesday morning.
Looking back, she weighed 15 lbs 12 oz at Dr. Perry’s office a week ago on Monday (one week prior to being admitted), so she may have been retaining fluid at that point too.
The night shift resident really rubbed me the wrong way last night. She came off as abrasive and you don’t get the feeling that she respects a parent’s input. For example, Ella was really fussy and it took a long time to get her to sleep. The resident came in and wanted to “listen to her”. That process wakes Ella up. Since she was saturating beautifully and there was nothing clinically to indicate a crises, we asked if she could hold off on listening. We got an attitude and she basically disagreed and said that she was going to listen to her anyway. Sure enough, it woke up Ella.
Fortunately, I’ve really liked the day shift team, so I’m going to focus my efforts in getting a plan in place today.
Please continue to pray that Ella will feel better. Also, that her and I can catch some naps throughout the day so we are not feeling so sleep deprived.
UPDATE – 10:30PM (MST): Thank you for all the prayers. Ella and I did catch a few short naps today and they definitely helped! Also, I think that Ella is so tired that she has actually been sleeping really well this past hour or so. I hope that is indicative of how she will rest for the remainder of the night.
Today was mostly a resting day for the Bun. They have left her on 1.5 liters of oxygen, but she has been stable and saturating beautifully all day long. I am sure that they will wean her at some point this evening or first thing in the morning.
She has gotten dry – this is why she is starting to feel better. The increased dosage of bumex and the shot of IV lasix has helped reduce her fluid. Her BUN on Monday was 14, it was 19 yesterday and this morning, it shot to 28 which is really dry. I think the increased diuretics along with the steroids have done the trick. In the past, we have only used diuretics and it has taken several days for her to dry out. The steroids shortened the life of that real quick, which is great because it means that Ella must be feeling better. She certainly isn’t laboring as hard to breathe.
Her swallow study is scheduled tomorrow. We should also hear back from pulmonology and gastroenterology regarding the next steps that we want to take with her care. Today was a lot of me pushing buttons and becoming a squeaky wheel to get them to understand that we need a plan. I think the pieces of the puzzle will start coming together tomorrow and the picture will be more clear about next steps.
Josh is working late tonight, but will be reliving me at some point. In the meantime, I’m going to shut my eyes and catch some zzzs right now. Later, I will dash home and sleep in our bed to get caught up on sleep and Josh will stay overnight with Ella.
Please pray that Ella sleeps well tonight…that will make for a much happier Daddy. Also, that we can consult with the various departments tomorrow and get the wisdom from all the doctors so that we can come up with a plan for Ella….a plan that we will feel comfortable with implementing.
Thanks again for all the support and prayers.

|
|
|
|
| |
|
|
|
Posted ( jooosh) in All Posts on August-7-2008 |
|
|

Yeah…that’s what I said…surgery. You can see by the look on Ella’s face she’s not too excited either.
I’ll get to that in a minute, but first let me bring ya’ll up to speed. Although I had a work project and couldn’t get to the hospital ’till midnight, I gave Tina a break so she could go home to sleep while I spent the night with Ella.
Once again the prednisolone kept Ella up pretty much all night. She was restless and woke up about every 15 minutes. She finally went to sleep around 5:00am but only for about 45 minutes or so.
Her oxygen was also weaned down to 1 liter last night, and she seamed to be tolerating it ok. She took a long 3 hour nap in the late morning and during that time her heart rate and saturations looked great. Her heart rate hovered around 105 bpm and even dipped as low as 89!
Later in the afternoon Ella started having some problems breathing. Her breaths became more labored and she started getting upset. I let the nurse know what was going on and we began to increase her O2, both in her cannulas and with blow by. Ella had a real hard time recovering but she finally did. We think we figured the cause of this one though. We believe that Ella’s O2 is being weaned too fast.
When she was on a liter of O2, her saturations hovered in the mid 90’s but would dip into the low 90’s as well. When this would happen her body would try and compensate by working harder to maintain the higher saturation. By the afternoon, she was just worn out which caused her to spiral down. We know Ella likes to take her time with things, so moving forward we will be weaning her slooowly so we don’t encounter this again.
Also, Ella had her swallow study done. It wasn’t real bad, but it wasn’t perfect either. The good news is that she is not aspirating immediately when she swallows, but her timing is off enough to where the food is being stopped by her vocal cords and muscles in her throat instead of the epiglottis. We’ll find out in the coming days the recommended approach for giving her food and drink orally.

Ella had an EKG done this evening just as a precautionary measure because her heart rate monitor kept throwing these weird alerts. The doc didn’t think she was actually experiencing them, but just to be on the safe side, she wanted a test done.
The big news of the day though relates to the upper GI study they did the other day. If you remember, the technician told Tina that everything looked ok. But after the radiologist studied the images in detail, it looks as though Ella’s nissen has pushed past her diaphragm and is up in her chest area. This is the most likely cause for her increased retching when she drinks or starts to cough because it’s pressing against her esophagus.
Repairing this will require surgery…something we’re really not excited about to say the least. We still have not talked about all the details with the surgery team, and we’re also waiting to get a consult from Dr. Kays before we do anything. The earliest the surgery would even take place would be the middle of next week, but we’ll just have to see. I just know that with all of Ella’s history, no surgery is going to be very straightforward.
Even with all this, Ella is taking it in stride. She’s seems to be feeling better tonight, even acting more like herself.
Please pray for our girl in the coming days and for wisdom so that path is made clear for the doctors and in our decisions.
Praise God for this sweet little Bun.
|
|
|
|
|
|