| |
|
|
|
|
|
|
|

…I love ya tomorrow, your always a day away.
Ella was up again all last night. She finally went to bed at 5am and we both slept until about 7:30am. I’m hoping that tonight is better, but I don’t think it will be. Those steroids do a number on her. They will be over in a couple of days – thank God.
Today was a good day for Ella. She made steps in the right direction. Her oxygen was at 1.5 liters most of the day and she remained stable. I decided to take over the weaning of the oxygen. I felt like they were weaning too fast and I could start to see the signs early when they were being too aggressive. Right now, Ella is taking a nap (I just fed her and administered the steroids so they have not kicked in yet!). Since she is sleeping, she is totally relaxed and requiring less oxygen. She is at 1 liter and saturating 100%, which is good. I expect that I will have to increase the oxygen while she is awake and fussy tonight, but I can tell that she is getting stronger. It will just take her awhile to get lower on her oxygen requirement. The good news is that we don’t have to stay in the hospital to make that happen.
She was poked again today for her labs. All her levels were reasonable, including her BUN which was 23. So, her BUN went from 14 on Monday to 28 on Wednesday (after being given megadoses of IV lasix and Bumex), and was 23 today on Friday after adjusting her Bumex dose for her weight.
The other observation: since she really dried out over the past day or so, she has not had a lot of secretions. We were getting to the point where she was having such thick secretions frequently and she did not know how to manage them. Therefore, she would cough, gag, retch. She was doing this 10-40 times per day. The interesting part: she has not been retching hardly at all since she has dried out.
Ella has been letting me know the past 2 days that she is dying of thirst. Finally late today, we got the okay from pulmonology to give her 4-8 ounces of water per day, as she desires. It’s been hard because I have been unable to give her anything via mouth. Yet, she is asking for it by opening up her mouth wide and complaining. Along with it being dry in Denver, the steroids can cause dry mouth. As soon as I could today, I gave her some water. She was a happy girl; she wanted it so bad. She took 4 ounces without a problem. Another highlight: she never retched. She has been retching with oral intake of fluid for the past few weeks, so it was very promising to see. Could this mean that retching is tied to secretions which is better/worse depending on how wet/dry she is at any given moment? Hmmm…
Grandpa visited her today. He has been tired too, so I caught him catching a few zzzs while I was talking to the in-house physical therapists.

As long as Ella can remain stable tonight, even though she is at a way higher oxygen requirement, they will discharge us tomorrow! This means that we can go home, let Ella get better and slowly wean the oxygen as we see necessary. Josh went out of town this evening and will be back late Tuesday evening. He was a bit hesitant to leave his girls, but I convinced him that we would be okay. Plus, we have Grandpa and lots of friends we can call on if we need help.
With a discharge from the hospital, it will mean that we have to come back to the hospital early next week for labs again. They will want to check all her electrolytes as well as her BUN to make sure that she is staying dry on her increased dosage of diuretics.
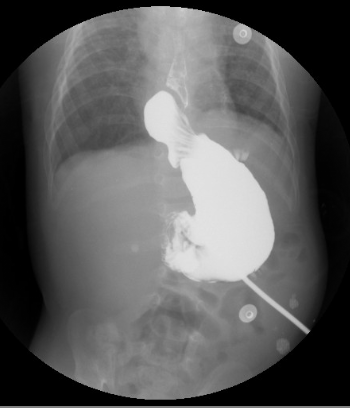
After speaking with the surgeon tonight, it is looking like we will need surgery to repair Ella’s nissen. If you remember, she has a nissen fundoplication (she underwent a surgery that took the upper part of her stomach and wrapped it to the lower part of her esophagus. This is a permanent surgery that was completed last Nov 2007 and was done to prevent her moderate to severe reflux as well as help prevent aspiration).
The upper GI results from the other day show that she has a hiatal hernia.
Mayo Clinic describes it this way:
“The exact cause of hiatal hernias isn’t known. Your chest cavity and abdomen are separated by your diaphragm — a large dome-shaped muscle that’s responsible for a major part of normal breathing. Your esophagus passes into your stomach through an opening in the diaphragm called the hiatus. Hiatal hernias occur when the muscle tissue surrounding this opening becomes weak, and the upper part of your stomach bulges up through the diaphragm into your chest cavity.”
Her nissen wrap has migrated above her diaphragm into her chest cavity and is currently pushing into the side of her esophagus, thus causing difficulty swallowing, gagging, retching and a potential over time to begin causing reflux.
This is not a surgery that is critical and needs to be done ASAP. We should wait until Ella is stable with her lungs and fluid issues. But there are consequences for waiting too long: the hiatus hernia can get bigger and portions of the stomach can migrate into the chest cavity too. Also, it is likely that Ella will continue to have the cough, gag, retch and swallow difficulties. They don’t really want us to pursue oral feeding therapy until it is repaired. With this in mind, we should consider having surgery in the next few weeks.
We are still waiting to get a second opinion from Dr. Kays. Based on what the surgeons here are telling me, she does not have a subtle hiatal hernia. It is easily noted on the radiology images and therefore, it is likely that Dr. Kays will agree with their recommendation(s).
Again, please pray that Ella continues to go the right direction and that she can strengthen. We would really like to go home tomorrow, if possible. Also, that Josh and I will have wisdom and discernment to make the right decision for Ella concerning her surgery, down to every detail.
Lamentations 3:22-23
Because of the LORD’s great love we are not consumed, for His promises never fail. They are new every morning; great is Your faithfulness.
|
|
|
|
| |
|
|
|
|
|
|
|
Man, this hospital is nice…and the views aren’t bad. A nice touch when you are pondering things and going through something heavy.
We left the hospital about 2pm today. Yippee! It is good to be writing this post from home this evening.
Ella did incredibly well last night. She slept solid the entire night. I thought the steroids would keep her up for a 4th night in a row, but I was pleasantly surprised. She slept from 9pm – 9am; I am sure she was exhausted from her lack of sleep these days too. I slept from 11pm – 6am, but those 7 hours felt like a dream!
Wow, I am not sure what happened. But Ella’s heart rate last night and this morning while she was relaxed and asleep were the lowest numbers I had ever seen. The only time the numbers have been even remotely close is mid-January in the NICU after they introduced sildenafil for the first time. This morning, I had to take a video so I can prove it to Josh. Her heart rate was fluctuating between 85-105. I have never seen them dance in the 80s before, ever. I knew that meant that she was very relaxed and had to be feeling better.
About 9pm last night, I weaned her oxygen down to 1 liter. She usually saturates incredible while she is sleeping – – it is always the awake time that is more dicey. But this morning, she was saturating well on 1 liter while awake too. Some might have argued to keep weaning, but I think the key with Ella is slow. So, we will likely stay on a liter for another 2-3 days. I want her to be rested and ready. Because we have not established a true baseline for oxygen requirement in the altitude and we want to be more on top of it, we may have to use a pulse oximeter during the daytime too so we can monitor and adjust accordingly.
We ordered a DVD from Shands to upload all of Ella’s medical records into the system at the Children’s Hospital in Denver. Unfortunately, they were having a tough time loading the images into their system. Josh tried viewing the images on my computer and it worked. Since I had the images handy, I thought I would show everyone some images that relate to this recent hospital stay.
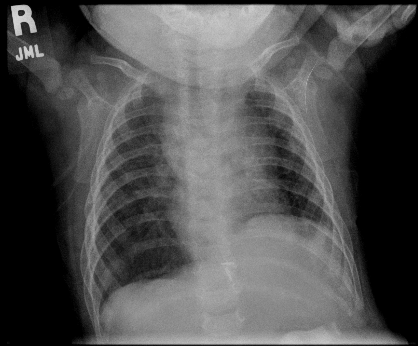
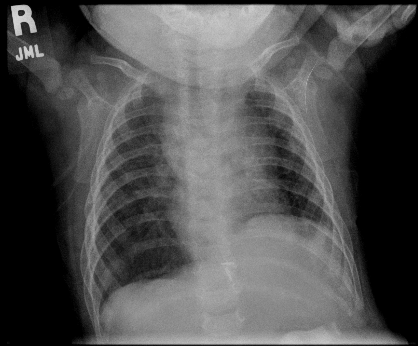
This is a picture of Ella’s lungs back in mid-May right before we left Gainesville. She was more “dry” during the time of this xray.
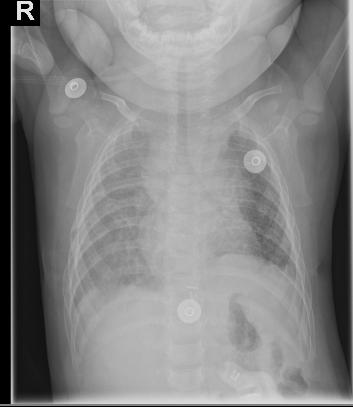
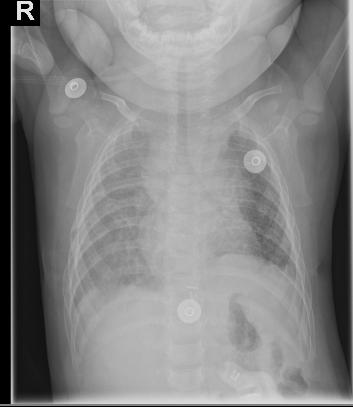
Below is Ella’s chest xray from Monday, August 5th when she was admitted to the Children’s Hospital. You can see that the film is hazy. This is what Ella’s lungs look like when she retains fluid and is more “wet”.
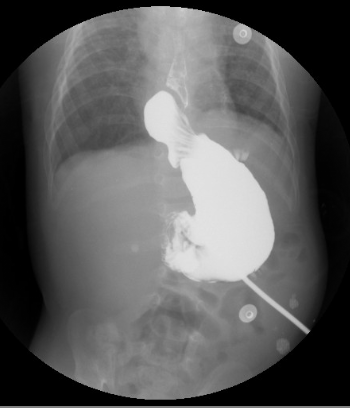
Also, below is a picture of Ella’s hiatal hernia. So you can see her stomach filled with the barum fluid that radiology uses for contrast. Above and to the left, the round ball shape is the nissen fundoplication or nissen wrap (where Dr. Kays tied the lower part of her esophagus to the upper part of her stomach), to prevent the reflux back into her esophagus and prevent aspiration. While the wrap still looks intact, it has herniated above into her chest through the hiatus (the natural opening in the diaphragm where the esophagus lies). So now it is above her diaphragm area resting in her chest against the side of the esophagus. This is why they think that she might be gagging and retching more than normal.
Speaking of retching, she has not retched a single time today! Again, she is more dried out and I don’t hear her wrestling with any secretions, which is a nice change. I would love it if we could keep her dry enough to not have to battle constant secretions.
Ella is sure feeling more like herself today. It’s so nice to see those smiles!
Another day has gone by without hearing from Dr. Kays. All I can think is that he is super busy. I’m hoping to hear his thoughts soon.
Our neighbor showed our house for rent this evening (and continues to mow the lawn for us – they’re saints!). We’re still praying for the right tenant to occupy our home. We know that He has a plan…we’re trying to be patient and trust.
Finally, thanks for all the prayers. The support means so much during times like this past week.
James 5:11
As you know, we consider blessed those who have persevered. You have heard of Job’s perseverance and have seen what the Lord finally brought about. The Lord is full of compassion and mercy.

|
|
|
|
| |
|
|
|
|
|
|
|
Today was a relaxing day at home with Ella.
She did really well last night sleeping in her own bed. Our pulse oximeter showed similar saturation and heart rate that mirrored the hospital. This is one of the best ways for us to keep a close watch on Ella’s fluid levels. Last night, she was saturating 100% and her heart rate was between 85-105 when she was in deep sleep. She is still on 1 liter of oxygen. If she does well tomorrow, I think we will look to wean tomorrow night again, once she is asleep.
As I type this, it is raining really hard in the metro Denver area. There is lots of thunder and lightening. I hope it does not wake up the Bun. It is very loud; it has made me cringe a few times. When I ran into her room to shut the windows, her saturation was 100% and her heart rate was 92. This is really good and so different than the week prior.
In the midst of Grandma West visiting and then going to the hospital, I neglected to mention about Ella’s therapy situation. We have been going through the Early Childhood Intervention program for OT and PT. Well, the OT that was assigned came for 2 appointments. By the last appointment, it was evident that it was not a match. I’m sure that she was very qualified, but she rubbed me the wrong way. Personality-wise, she had an abrasive edge to her. So, I asked our case manager if we could find someone else in their network to work with Ella.
Then, last Saturday before we went to the hospital, Ella’s PT called and explained that she had a personal situation arise and needed to cut back her work schedule. So, she dropped us off her schedule. Along with needing to thin out her schedule, I also think that Ella was a lot of work and a great challenge for this therapist. We really liked her, so we’re bummed that we have to find another one.
We started this process when we came back on June 1st. Two months have passed and Ella has not really gotten any great therapy sessions. We have not made any progress forward for Ella for OT or PT. I just feel like we made such great progress in the 4 months post-hospital in Gainesville. Now we are having a tough time getting into a groove for therapy in Denver.
I am planning on getting services through the Early Intervention Program, but have decided to pursue therapy through our health insurance benefits again too for the majority of the sessions. I just feel like the therapists are way better and more experienced. It is strange to me that we ended up with 2 great therapists in Gainesville and now that we are back home in Denver (in a major metro area), we are having trouble making this happen.
Also, I mentioned before that we were trying to get private duty nursing hours. A few weeks back, our health insurance company authorized 20 hours per week for the first 30 days and then re-evaluate. We have been through 7 health care agencies and no one can staff. There is such a shortage in certified nurses through the health care agencies, especially those that work with pediatric patients. So, we have not been able to take advantage of this benefit. Hoping and praying that it will work out, if it is meant to be. It would be nice to have a break here and there.
I made contact with some NICU nurses today and found out that Dr. Kays is on vacation. He is not expected back until August 18th. So, we will need to be patient and wait for his opinion.
Listening to Charles Stanley this afternoon, I am reminded of four truths about God. First, that God is in absolute control. He controls all the circumstances in our life. Second, He will always meet our every need (things that fit into His will and purpose for our lives). Third, God is always with us (nothing will ever be able to separate us from the love of God). Lastly, that He loves us eternally. All of these truths mean that even when the circumstances of life are not the best, we can have confidence.
Please continue to pray for Ella and her health – that she will remain strong. Also, that the best therapists will be placed in our path. And finally, please pray for our upcoming decisions regarding her surgery.
Psalm 68:19
Praise be to the LORD, to God our Savior, who daily bears our burdens.

|
|
|
|
| |
|
|
|
|
|
|
|
It was another great day with the Bun.
We took a field trip down to the Super Target near the house. We are not really supposed to go inside with her, but it was a necessity. Since we were at the hospital last week and Josh is out of town, the refrigerator and pantry were empty. I could have likely eaten cereal for 2 days, but we were out of nursery water for Ella’s formula. So we took the plunge and walked to get some groceries. I opted to use the Baby Bjorn and give Ella a view of her surroundings. This way, the oxygen tank and groceries could be place d in the stroller on the way back.
It was a beautiful day outside, nice and sunny. Ella sported her navy dress with a cap and sunglasses. She looked adorable. It was great exercise for her to hold her head upright while we walked. Plus, it was unseasonably hot in Colorado for the past few weeks. So we have not taken a walk in a long time. Today, it was a normal temperature. The high was 88 and it has cooled down to 69 degrees this evening. It was nice to get outside with her again. I think she really likes it.
We heard that a new PT and OT have been assigned to us from Developmental Pathways. It will be interesting to see how things go over the coming weeks with the new therapists. And although it will not be quite as consistent, we are still going to try and pursue a different PT and OT through a home health care agency too. Between therapy from both angles, we should be able to give Ella what she needs.
Tomorrow, we get to go back to the Children’s Hospital for blood labs. They want to check all her electrolytes and other levels. It will be interesting to see where her BUN falls. I think it might be a tad lower than the last draw which was 23. But we’ll see.
Once we’re done with labs, we are going to see Dr. Perry. We haven’t seen him since a week ago. He went out of town last week, so we did keep in touch with colleagues from his practice. But it will be good to see him again and come up with our plan for Ella over the coming weeks.
When I put Ella to bed tonight, she was still on 1 liter and saturating 100%. I may try weaning her oxygen once she is really asleep. This way, I can see if the extra oxygen is truly making a difference. It seems like she might be ready to go down a little bit since she has been at 1 liter for 3 days now.
The picture below is so cute. This was earlier in the evening when she decided to take a snooze. I just love how relaxed she is and that she likes to cross her legs, even when she is catching up on beauty sleep.
We’re missing Josh and can’t wait for him to come home.

|
|
|
|
| |
|
|
|
|
|
|
|
Our day seemed to pass quickly.
In the afternoon, we headed to the Children’s Hospital for lab work. It took a second nurse to try sticking Ella. Yuk – – I just hate having that done. And Ella can spot it coming and she holds her breath and cries really hard. She has been stuck so much in the past week or so. Her feet, hands and arms are bruised from needles. Fortunately, we get a little break. The next time we need labs will be a week from Thursday, on August 21st.
Her labs from today looked good. Last week, they had to give her more potassium. But today, everything was in normal range and her BUN was 29. So, she is staying dry. Along those lines, we have not had a single retch in days. I had never made the association of retching with her pulmonary edema status (being wet or dry), but I think the two are closely tied together.
We visited with Dr. Perry this afternoon. He had been out of town since last Tuesday and so we were catching up on all the details. Ella decided to take a snooze while we were talking about everything.
We have two conflicting reports on nutrition, one from the independent consultant that came to our home 2 weeks ago, the other from the nutritionist at the hospital. One thinks she needs more calories, the other thinks everything right now is fine. Dr. Perry is going to do his own calorie calculations and get back to me in a couple of days.
Tomorrow, there is a case manager coming to evaluate Ella to see if she can qualify for the Medicaid waiver program (qualify for Medicaid based on her own income which is zero). The wait list is 1.5 years, but first they send someone to verify and make sure that she qualifies based on her medical condition.
Ella enjoys playing with her oxygen tubing. Quite honestly, I’m not sure what she will do someday without the tubing!
Speaking of oxygen, I tried weaning Ella down to 750ccs last night. She seemed to be okay while sleeping so I left it overnight. Throughout the day, she almost seemed like she might need more, but her color was okay and she was behaving fine, so I left it. When we were at Dr. Perry’s, they tracked her at 96-97% saturation and heart rate between 155-165. That is so much higher than what it had been previously.
When I got home, I tried putting her to bed at 750ccs, but her heart rate seemed to be high. So, I tried increasing the oxygen. Right now, she is at least a liter, closer to 1.5 liters (tough to read the exact amount on the concentrator we have right now). However, her heart rate is still high. I’m not sure why it is so much higher, even compared to the last several days. Maybe keeping her on a lower oxygen amount for too long is causing her some grief? Typically, a raised heart rate simply means a fever or that she is working too hard. Right now, she does not have a fever so I am left to believe that she might be working too hard. It is such a guessing game – finding the right oxygen level.
But we know that God has a plan. Some days it is hard to remember that truth.
Psalm 145:8-9
The LORD is gracious and compassionate, slow to anger and rich in love. The LORD is good to all; He has compassion on all He has made.

|
|
|
|
| |
|
|
|
|
|
|
|

Yes, tachycardiac means rapid heart rate. I don’t normally post in the middle of the day, but felt it was worth letting everyone know where we stand. So, if these events seem sudden, you may want to catch up by reading last night’s post.
The night was okay except that her alarm was going off intermittently due to an elevated heart rate. I noted this before going to bed and when the alarm would go off throughout the night, I knew before walking into her room, that her heart rate was the culprit.
It is strange to see such a high heart rate. She was on 1 – 1.5 liters when I put her to bed. It is tough to know the exact amount because the dial on the oxygen concentrator. Since it goes up to 5+ liters, the lines of differentiation even between 1-2 liters are slight.
She leaked out of her diaper this morning, so I guess she had good urine output. After cleaning up her bed and changing her, I laid her back down. She seemed fussy. Her heart rate was around 175. As soon as I laid her back down at 8am, she went back to sleep for another 1.5 hours. While she was fast asleep, I would peek in at her. Her saturation was fine, 98-100 but her heart rate was around 155. It stayed this way all last night and is higher than her baseline.
When I woke her up at 9:30am, she was acting like she didn’t feel great. As I brought her downstairs, I kept the pulse oximeter attached to her because I felt like I needed to watch her closer today. Also, since the oxygen concentrator was not exact enough for me and I couldn’t tell exactly how much O2 she was getting, I switched to the portable oxygen tank.
Around 9:45am after she had eaten, she was on 1 liter and her saturation dropped to the low 90s and her heart rate was fluctuating between 185-205. There is no half marks on the regulator, so I increased her from 1 liter to 2 liters. That seemed to help decrease her heart rate, but it is still too high.
Later around 12:15pm, when she was down to a heart rate of 145-165 while just laying there watching a video, I tried taking her back down to 1 liter. Within 30 minutes, she was back saturating in the low 90s with her heart rate at 185. So for whatever reason, I have to believe that extra oxygen is helping her work a bit less.
Besides watching her like a hawk, I have spent most of the morning on the phone. I called the pharmacy checking her sildenafil that was refilled a while back. This was Josh’s idea. I asked if the properties of the compound could break down at all. In other words, was her med not working right? I wanted them to verify that they mixed it correctly and to let me know if the sildenafil could break down. For example, there was about an 8 hour period where it was not refrigerated. Would that affect it? Basically, the pharmacy stated that the prescription should be fine, it would take much longer to break down.
Well, that was one variable out of the way. I called to run her symptoms by someone at Cherry Creek Pediatrics (Dr. Perry does not work on Wednesdays). The triage nurse looked for another doctor around the office, for an opinion. Meanwhile, Dr. Perry called my home number. He told me that he would call regarding her food intake, as a f/u to our appointment yesterday. But I thought he called because the office informed him of her status. Instead, it was pure coincidence that he called this morning while all of this was going on.
I gave him all my thoughts, including the only variables that have changed are using our meds at home (but that the pharmacy was confident our meds were ok) and that we stopped the steroids. Also, I told him that I could hear congestion in her throat this morning for the first time since last Tuesday, when they gave her the megadose of diuretics. And therefore, she has had 4 episodes of retching, one where she spit up water she recently drank. This is the first time she has retched in a week. I hope the nissen isn’t causing more problems. We are trying to be patient and wait for Dr. Kays to come back from the Cayman Islands. Dr. Perry told me to hang tight – he wanted to call the pulmonologists at the Children’s Hospital.
He called back after talking with Dr. Kerby, one of the pulmonologists that watched Ella last week in the hospital. They reviewed everything and sure enough, they are all scratching her heads. This should make Dr. Kays feel better – – it is not just him. Ella is just not textbook about anything!
All her labs look fine and based on her clinical signs, they just want us to watch her closely over the next 24 hours. Dr. Kerby said that sometimes there can be a rebound effect once you stop the steroid treatment. Although nothing really points to why her heart rate would be elevated.
As long as we are able to work with 2 liters and below, they are fine with us managing the problem from home and not at the hospital. If things worsen and she requires more than 2 liters, I am directed to call the pulmonology clinic at the hospital directly. Otherwise, Dr. Perry and I plan on talking in the morning. If the elevated heart rate has persisted and not gotten better by tomorrow morning, they will likely see if they can fit me into a slot in the outpatient pulmonology clinic.
As far as food and his caloric calculations, Dr. Perry thinks she needs more calories. This is consistent with the evaluation from the nutritionist that came to our home. He reviewed the calculations that the nutritionist provided from the hospital and noted that they were off. Rather than increase the density of the food, he wants to increase her fluid intake. He feels okay doing that considering how dry she is with the BUN being 29. So, we are going to increase her food intake by 20ccs each day for the next 5 days. This will give her more calories to help with true weight gain. Let’s hope Ella tolerates it!
Right now, it is around 2:30pm and Ella is taking a little snooze. She is on 2 liters and her heart rate is fluctuating between 125-145, which is better to see. Again, this is still higher than normal, plus she is on a lot more oxygen.
Please say a prayer for Ella today…that she would feel better…that the doctors will be able to figure out what is plaguing her little body.
And as a side note, Josh missed his flight last night, so he had to wake up at 4am this morning to catch the earliest flight and then drive straight to work. So we haven’t seen Dad at home yet, but we should this evening.

|
|
|
|
| |
|
|
|
|
|
|
|

Unfortunately, Ella is about the same.
Last night while she was sleeping, we were able to adjust her down to 1 liter of oxygen. Her heart rate was mostly between 125-135 which is manageable (still higher than normal).
Once she was awake, the 1 liter of oxygen was not enough. Within 30 minutes, her saturation went down to low 90s and her heart rate was up around 185. This is way too high and basically the same as yesterday.
When I spoke to Dr. Perry, I explained what was going on and he could hear the alarm from her pulse oximeter going off in the background. He noted that she might need more oxygen while she is awake and to go ahead and keep her comfortable, especially if the extra oxygen would help her heart rate to decline.
I tried 1.5 liters but it did not seem to make a difference. Once I switched her to 2 liters and waited, her saturation was 99-100% and her heart rate when resting went down to 150ish. This is more manageable.
Dr. Perry thinks that although her condition has persisted, we should sit tight and give her the O2 she requires to keep her comfortable. If she becomes fussy or exhibits other signs of distress or requires more oxygen than 2 liters, he wants us to call back. Otherwise, we will just plan to go to the pulmonology clinic at our normal scheduled appointment next Thursday at 3pm.
So even though Ella is “dry”, she did retch a few times today. Also, she still is requiring more oxygen even though she does not have pulmonary edema. The steroids made a huge difference for her last week. And somehow over the past 2 months, things are different for Ella. She seemed to be stable 24/7 on way less oxygen; not different amounts of oxygen at night versus the daytime. We were also at sea level. She was not retching post NICU in Florida the way she has since we have been home in Denver, but she also got more “wet”.
I may have mentioned last week that they want to do a bronchoscopy. Since Ella would need to go under general anesthesia, they want to do this procedure at the same time as her hiatal hernia surgery. Bronchoscopy is a procedure that allows the pulmonologist to look at the airway through a thin viewing instrument called a bronchoscope. During a bronchoscopy, they will examine Ella’s throat, larynx, trachea, and lower airways.
The pulmonologist last week mentioned that when they did the swallow study, that Ella’s epiglottis does not function properly to help avoid aspiration. Your body has one other built-in feature to help avoid aspiration and that is the muscles around your vocal cords. From her clinical signs, they think that Ella might have weak muscles around her vocal cords too, likely from being intubated for so long. This could explain difficulty swallowing, working harder to breathe (if the muscles are floppy and don’t contract properly, it blocks the airway), retching, etc. Also, it might mean that Ella could be micro-aspirating or is at greater risk to aspirate. So, they have not given us the thumbs up to move forward with any oral feeding until this test is complete.
This is another reason we are anxious for Dr. Kays opinion, so that we can figure out when to schedule the bronchoscopy and hiatal hernia surgery. Without these procedures completed, we cannot move forward with any feeding therapies.
It’s just hard to sit each day and wait for an entire week. We know something isn’t right because she is not really stable unless she is on 2 liters of oxygen when she is awake and 1 liter when she is asleep.
Please pray for the Bun and her comfort. Also, that her respiratory status would improve in the coming days. Finally, that we will be given wisdom on the right procedures for Ella and these latest medical challenges.
Nahum 1:7
The LORD is good,
a refuge in times of trouble.
He cares for those who trust in him.

|
|
|
|
| |
|
|
|
|
|
|
|

Ella seemed more fussy today.
When we woke up, her numbers looked good on 1 liter of oxygen, which is what she slept with overnight. But within 1-2 hours of her being awake and trying to breathe, her heart rate increased and saturation decreased. Sure enough, I increased her to 2 liters and she has been stable, no different than the past 2 days.
She has been more fussy – I can tell because it is hard to get a smile when she doesn’t feel great. Also, she seems to have a lot of secretions that she is trying to manage. The secretions started a few days ago and seem to be getting worse. This does not make a lot of sense considering that her labs on Tuesday showed that she is very dry and does not have any pulmonary edema. But wherever the secretions are coming from, they are making her retch again, hard. That can’t feel good, so I’m not surprised that she is fussy.
It has been hard to get her to take naps today. She just seems extra fussy and uncomfortable. That is not a good sign, so I’m hoping that things do not worsen over the weekend, when less doctors are around.
Still looking forward to Dr. Kays returning on Monday to see if we can get an answer from him. I know he is going to be slammed when he returns, but I’m still hoping we will hear from him on Monday or Tuesday of next week.
We will be meeting our new PT on Monday morning. Although Ella will not be up for much work, I figured that she could come to meet Ella and take down her history. It’s always time consuming to start services with a new therapist, so I figured that I would get the ball rolling now. Our new OT called us too and has the first evaluation scheduled for Thurs, Aug 28th. So slowly but surely, those services from the Early Intervention Program will be in place. If you remember, we were only approved for services 1x per week for OT and 1x per week of PT. So we are still trying to also get OT and PT assigned through our insurance benefits too. Although it is not ideal to have multiple therapists, the more therapy, the better. We have so much catching up to do!
Please pray that Ella will improve over the weekend, and if nothing else, that we can continue to keep her comfortable until our pulmonology appointment next week.
Psalm 55:22
Cast your cares on the LORD and he will sustain you; he will never let the righteous fall.
UPDATE 8:45pm MST: Ella finally took a really long nap, like 3 hours long. She woke up with a smile. Praise God! Oh, and any thoughts on my fortune?
|
|
|
|
| |
|
|
|
Posted ( jooosh) in All Posts on August-16-2008 |
|
|

Ella is continuing to require 2 liters of O2 to maintain her saturations and a manageable heart rate. She exceeded 180bpm a few times this afternoon, but she mostly hovered between 150 – 160bpm. When she was sleeping last night, her heart rate fell closer to her previous baseline of around 115bpm. It seems that her tachycardic episodes are really occurring during the times she is awake.
Ella also had a few retching episodes today. These moments have been less frequent than the week before she entered the hospital, but even a few times a day is too much in my mind.
We hope to get more insight into Ella’s respiratory issues once she has a bronchoscopy performed. We’re planning to have this done at the same time she has the surgery to repair her hiatal hernia.
Even with her elevated heart rate and increased O2, you can see by the pictures that Ella is looking and behaving ok clinically.

While Tina was out, the Bun and I enjoyed some cuddle time together and I even got her laughing pretty good with some tickling.

We also had a college friend of ours stop by to see us and our girl. Ella made a point to bake her a patty cake.
Ella’s day of surgery is looming, but still not set in stone. I’m not trying to focus on it too much until it gets here. We know that we can trust the Lord in all things. The journey we have been on over this last year leaves us no doubt. Praise God for where He has us.
James 1:2-4 (New Living Translation)
Dear brothers and sisters, when troubles come your way, consider it an opportunity for great joy. For you know that when your faith is tested, your endurance has a chance to grow. So let it grow, for when your endurance is fully developed, you will be perfect and complete, needing nothing.

|
|
|
|
| |
|
|
|
Posted ( jooosh) in All Posts on August-17-2008 |
|
|
Ella’s still seems about the same.
Until we can get the broncoscopy and surgery completed, we feel like we’re in a holding pattern. Ella is still requiring 2 liters of oxygen, has an elevated heart rate, is trying her best to deal with secretions via coughing and retching. We can’t try any oral food therapy. You can tell that she doesn’t feel great, so you hate to push her hard with physical therapy. Maybe the pulmonolgy appointment on Thursday will provide more insight, but we’ve been led to believe that they really need the broncoscopy to further diagnose what might be going on and how to further treat her symptoms.
We’re anxious to hear from Dr. Kays. He’s supposed to be back at work tomorrow. We just want his opinion on the proposed surgery and to see if a doctor-to-doctor consult is recommended.
The highlight of the day was Grandpa visiting and treating us to Mexican food for lunch while the Bun consumed her Alimentum. And of course, Ella resting on me was pretty cute too.
Also of note: Today was a bit of a special day. It marks the time in my life when I have now spent more time with Tina than without her. I was 17 years, 11 months, and 13 days old when I asked her to be my girlfriend. Today, Tina and I have been together 17 years, 11 months, and 14 days.
Praise God for all He does and continues to do in our lives.
Psalm 71:14
But as for me, I will always have hope;
I will praise you more and more.

|
|
|
|
|
|