| |
|
|
|
Posted ( jooosh) in All Posts on April-16-2010 |
|
|

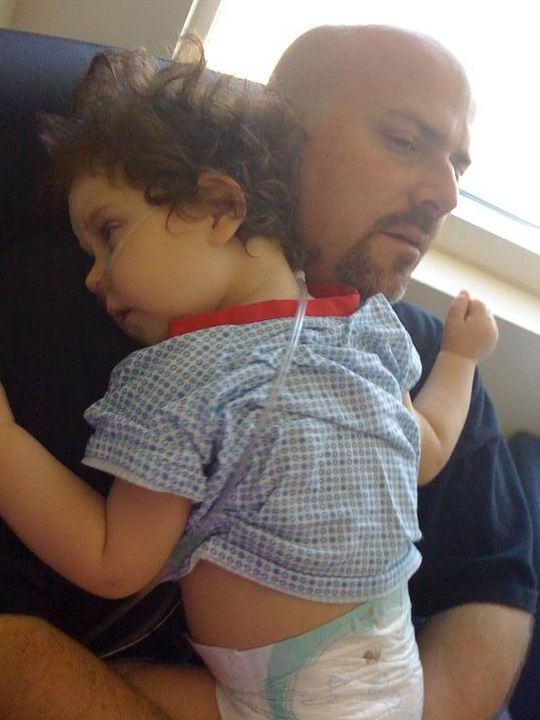
At the moment the kiddo is resting. She’s been doing a lot of this the last day. AS a matter of fact, since last night around 10pm and it is 5:30pm today and she has not stopped sleeping. I think it’s a combo of her body wanting to rest, plus the bevy of meds that are making her sleepy. I’ll tell you though, I’m happy to have her sleeping considering the alternative. Seeing your kiddo go through narcotic withdrawal symptoms is one of the hardest things I’ve ever had to watch.
She shakes and babbles and doesn’t act like herself plus she is so itchy. It’s really heartbreaking and scary at the same time. There’s also no way to know for sure how much longer it will last either. I mean, the symptoms will go away eventually, but it could last even another week! She has some moments of lucidity when the methadone and ativan hit her just right, but it’s not all the time yet. So keep sleeping sweet girl.
On a more positive note, Ella’s bowels are moving along. She had her first poop last night (yay) which is always a big deal after surgery, let alone bowel surgery. They docs are pushing to switch all meds to PO (by mouth/g-tube for Ella), and so far Ella is processing them in her tummy just fine.
We had an unofficial confirmation of this when she had her echo done. The docs had the NO (nitric oxide) stopped and checked her heart to see if the sildenafil was now working instead for her pulmonary hypertension. Peeking over the tech’s shoulder, he confirmed that her echo looked good compared to the previous one. Yay for Ella’s body moving forward! If Ella keeps this track, the next steps will be introducing food back into her system. The rumor is that a very slow drip of food into her g-tube might happen as quickly as tomorrow.
One small bummer is with all the positive steps forward, there’s a good chance they’ll move us out of the PICU. For Ella it’s a good thing, but for her parents it’s going to present some challenges. The regular rooms are shared, which isn’t an issue, unless some kiddo comes in with some major cold putting Ella at risk. They’re not supposed to put kids like this in a room with Ella, but they do. Plus, no couch/bed to sleep on, so we’ll* probably be catching our winks in a chair. Here’s hoping that somehow we can be discharged right from the PICU, but I have a feeling that won’t happen.

Ella’s Grandma West came for a visit yesterday evening. She made Ella this beautiful blanket and matching cover for her frog pillow. Grandma West got to see Ella during one of her more lucid moments, which was enjoyable for both.
Please continue to pray for our sweet girl as she progresses forward. The support that you all have given to us over the last week has meant so much. It really carries us through these times.
P.S. Lola the pooch is still sick. Hoping her antibiotics kick in soon.
*By “we’ll” I mean my saint of a wife who has been staying next to Ella every night so far. Sleeping on a chair stinks so I may be pushing her to sleep in the rig a couple nights so she can catch up.

|
|
|
|
| |
|
|
|
Posted ( jooosh) in All Posts on April-17-2010 |
|
|

Last night was hard. The medicines to help treat the narcotic withdrawal symptoms plus the itchy symptoms were being administered once every 3 hours. It seems like Ella has already built up a tolerance because at 4am, she could not stop itching and wiggling around the bed. Unfortunately, they could not give her anything to help with the relief. She was wiggling and upset till 6am, when they gave her more meds.
This behavior was shared with the doctors. With this in mind they decided to give a half dose of morphine in between the other meds to possibly help with the withdrawal symptoms. The nurse gave the first dose this morning, and unfortunately, it did nothing for her. One of the docs came by and saw Ella having another episode in the afternoon. They decided to up the dose of morphine hoping it would help. We haven’t use it yet, but there’s a good chance we will have to later.
Tina and I are upset that they have to pump Ella so full of these other meds just to help her recover from the withdrawal symptoms. Even once the symptoms calm down, we’ll have to wean her off these other meds. Granted, we won’t need to be in the hospital to do this, but it could still take up to 6 weeks to titrate the methdone and ativan! Uhhhh…such a bummer.
Ella had a echo done yesterday, but we didn’t hear the definitive results until today. It looked the same as when she was on the NO (nitric oxide) showing mild pulmonary hypertension. This means that the current dose of sildenafil isn’t working like it normally does for her. Our guess is that it’s being absorbed in the stomach but not in the small intestine, minimizing the impact. The docs ordered an increased dose for now until her small intestines are back in line. Hopefully this is all it takes to get her pulmonary hypertension back under control.
Tina also reminded the docs during rounds that Ella was on a regular dose of Miralax at home. They admitted forgetting this fact and wrote an order for her to be put back on it. As of this time, there’s no set date on when we get to start feeding her. The surgery team came by and confirmed that we should still hold off on the food for now. The head surgeon listened to her bowels and, just by the sound, was able to tell that she’s still too distended and not ready. He also affirmed that all the other meds we’re giving to minimize Ella’s withdrawal symptoms will slow down her motility as well. So for now the kiddo is on a steady diet of TPN and lipids via her IV.
With all the complications still in the way, it doens’t look like we’ll be moving out of the PICU for a bit. I guess we’ll consider that a silver lining.
Thanks to all of you who have brought us dinner, sent cards, delivered gift baskets, and visited. The greatest blessing of being in California during this time is the fact that family and friends can support us with their physical presence. Your amazing love, support, and prayers keeps us sane. We also appreciate all the virtual love and support from our friends and family across the country. Thanks for being here with us!
Please continue to pray for our sweet girl…that her withdrawal symptoms will subside, her body will heal, and the Lords work will be done through the circumstances he’s having us go through.
Thank you Lord for bringing us here and for carrying us through this incredibly challenging time. We know you’re in control, and we trust in you, but it is hard to see your child go through this. We know you, Father, can relate. Jesus, we ask that you comfort our child and reduce her withdrawal symtoms. Heal her body, and make her whole again. We praise you Lord for the precious child you’ve blessed us with. Thank you for her. We love her so much. Amen
|
|
|
|
| |
|
|
|
Posted ( jooosh) in All Posts on April-18-2010 |
|
|

We’ll give a quick update, but with all the not so fun times we’re experiencing now, we figured a photo break escape for you Ella fans would be good. But first…
Ella’s hanging in there, but the parents are exhausted. Her withdrawal symptoms have lessened a little bit, but she still very spacey and itchy. She slept through the night and had a good morning. She was awake for about 2 hours last night and then has been for most of today although she is still sedated. We have tried not to give any additional doses of morphine and have been able to avoid it thus far. One surprise today: she actually tried to sit up in the bed even though she didn’t have the balance or strength to sit on her own! That is her fighting spirit trying to work through the withdrawal meds!

Surgery came by to take a look at her: they still wanted to hold off on food. Once we heard the news, the PICU team thought it might be good to try her withdrawal meds via her g-tube versus IV. A small change, but one in the right direction (since we will have to wean the withdrawal meds at home too). However, they gave methadone via g-tube and within 10 minutes, she was writhing in pain. Apparently, her tummy really hurt. We vented her belly as much as possible and after 15 minutes, she was content again. So, they had to order the withdrawal medicines via IV again.
Ella’s hand looked puffy at the IV site and although it was still flushing, it had been active for 10 days. So, we were able to take it off today to give her hand a break. We checked the central line to make sure that we could still draw labs and it appeared that there were clots in the line. They ordered a TPA (tissue plasminogen activator) to clean up the catheter and eliminate clots. Fortunately, it worked and they are now able to draw off of two more lumens. Thank goodness!
We had asked the docs as well if they were sure that she’s experiencing withdrawal symptoms and not something else. With all the symptoms Ella is presenting though, we’re confident that we’re treating withdrawal. They have a Finnigan scale where they score her each day to see where she ranks on the scale. Ella is presenting most of the signs of true narcotic withdrawal. It’s so difficult seeing your kiddo deal with this when just a few weeks ago we were all enjoying our time together.

One more concern: this afternoon, she seems like her respiratory rate is higher, heart rate a bit higher and saturations not as good. Knowing Ella, it might be fluid related. She has been positive for urine output the past few days. Maybe the net effect is accumulating and we’re seeing signs of fluid retention. On a similar note, they increased her dosage of sildenafil because the echo showed that it was not all being absorbed through her g-tube. Maybe her diuretic is doing the same thing? If she continues this way overnight, we’ll likely be requesting a chest xray in the morning, just to eliminate that possibility.
Please continue to pray for the Bun’s healing and forward progress.
Below are some pictures of our trip since we hit California back in March. Enjoy…

Lovin’ on Grandma West
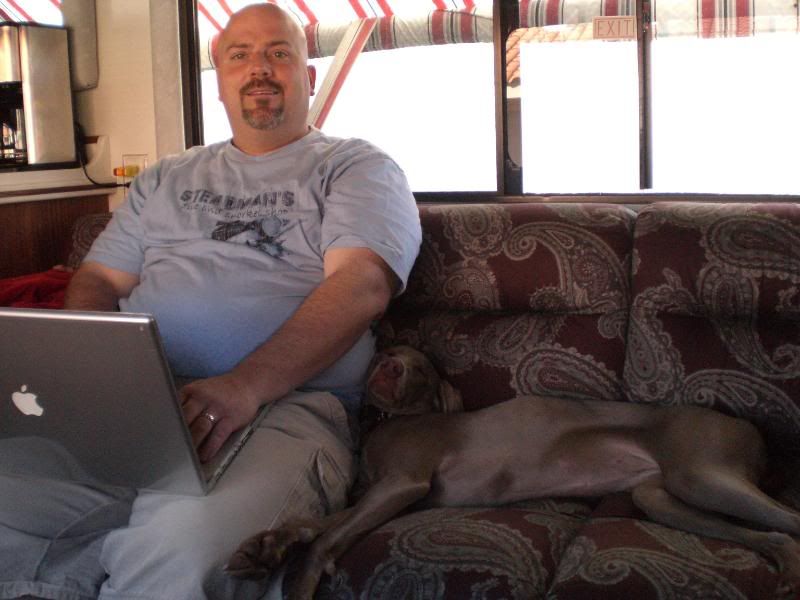
Ella’s dad and his asistant
Contortionist Pooch

Ahhhh…the Pacific Coast

Waiting in line

Nothing like a beautiful sunset to inspire black water dumping

The Rig

Rockstars!

Unnecessary extreme closeup self portrait

“Yay! Dad’s dumping the black water”

Don’t ask, Don’t tell

Even the pooch enjoys a good sunset

I’m givin’ it all I can captain…I think she’s gonna blow!!!

Ummm…semi-fresh water spray?

I have me some mad dumping hose cleaning skillz (ummm…are you wearing flip flops???)

How cute can you get?

Even cuter!

EVEN CUTER!

Standin’ up baby

Yeah…pretty stinkin’ cute!

Out in the stroller

A pooch and her Kong

Ella, “Can I have the Kong?”

Lola, “Yeah…no…I don’t think so!”

Pooch refill

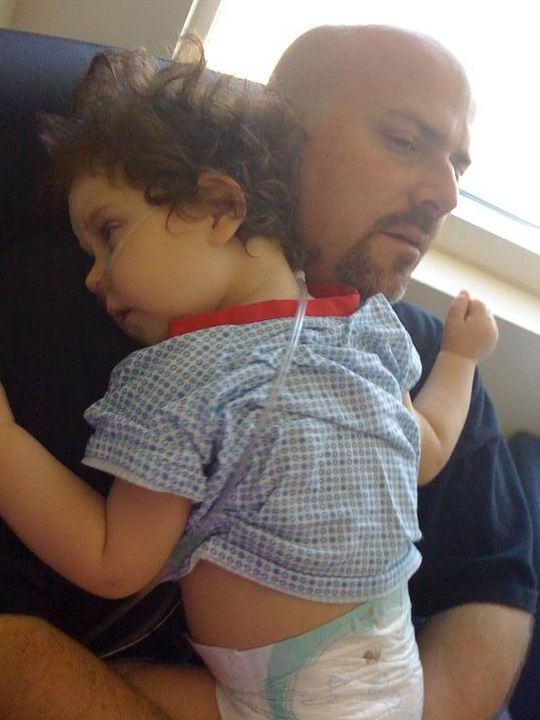
Restin’ on poppa

Diva dog pose

PCH in Laguna Beach

The beach in Laguna

Face to face with cousins for the first time!

Richard and Megan

Richard and Megan again

The whole crew

What’s goin’ on outside?
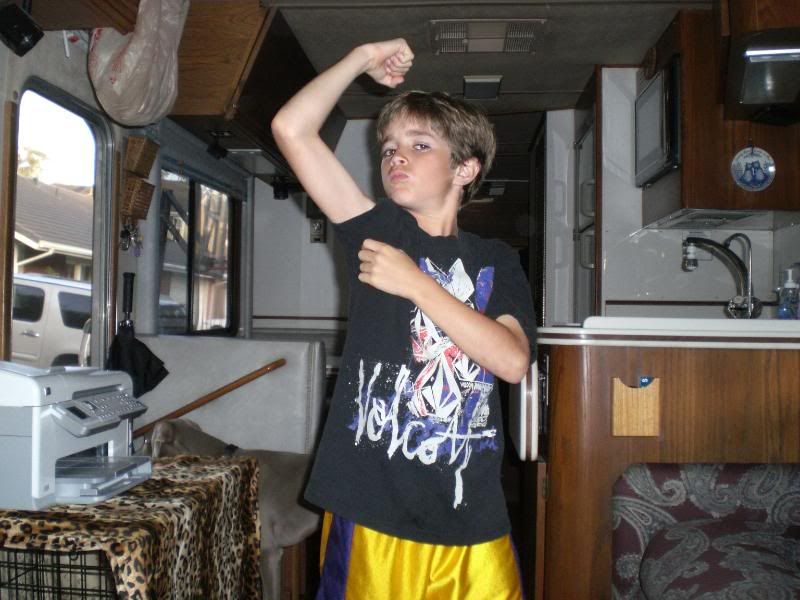
Excuse me sir, do you have tickets to the gun show?

Megan and Aunt Tina

A sleeping Lo

Cousins Claire and Ryan!

Sleepin’ Bun

Great Grandma and the pooch

Ella’s Great Grandparents

Silly Bun

Nap time

The Rig in front of the Great Grandparent’s house

O2 Pickup at Apria

Pooch walkin’ at Doheney State Beach

The parking spot

Lola enjoying the view…and…well…enjoying being a dog

Silly Dad

Cute Patoot

The smiles melt your heart

The melting continues

More cuteness

Just darling

Woah!!!

What’s this!!!!

Look Ma…no cannulas!!

West Family Self Portrait
|
|
|
|
| |
|
|
|
|
|
|
|

Remember on yesterday’s post how I mentioned that we were seeing Ella go in the wrong direction. I warned the resident during the day shift and they just wanted to “watch and see”. Later last night, it just kept getting worse. Ella had two episodes where she got upset and her saturations dropped into the 30s and she passed out on me – – twice! When this happened, we increased her to 2.5 liters and it still took a good amount of time for her to come back up. This pushed Josh and I to put on our armor and start war with the night resident. Although this particular resident had not been following her all the time, we pled our case: based on everything we know about Ella, she has to be fluid overloaded.
Then, we started asking for the facts since we’re not even convinced that she was dried out enough after surgery. How fluid positive is she for the past few days since you halted IV Lasix? We found out that she had been fluid positive 2 liters! That is the same amount as the day after surgery. Then, I asked about her weight which is another indicator. Remember when I mentioned that Ella lost weight? Well, she was 13.6 kilos three nights ago (29.92 pounds). Tonight, she was 15.1 kilos (33 pounds). She is on IV drips for nourishment, so there is no way that a 2 year old would gain 3 pounds in 3 days!
This is so frustrating. We feel like we are back at square one and that they are not listening to us about her fluid sensitivity. We had the same frustration initially in Denver until we were there for nearly 10 weeks! We are only at a week and a half, but this is painful.
After we discussed with the night resident, we negotiated one dose of Lasix at 8:30pm to see what would happen. Ella responded within the hour and peed out 178ccs. Next, we asked about another dose in 6 hours at 2:30am. At first, the resident only wanted to give a half of a dose of Lasix. That was not going to fly. Josh had already left for the night, so I put on my armor and had another discussion with the resident shy of midnight. I was able to negotiate another full dose scheduled at 2:30am. Before the nurse administered it, we changed a diaper with 95ccs. The dose of Lasix at 2:30am produced 378ccs of pee! She also had a chest xray this morning at 5:30am.
We will continue the battle with the day shift. Please pray that they will begin to listen to us about Ella’s physiology and her needs. She is not text book and they need to consider her specific needs, not the standard care of protocol. Our baby girl has so many things to recover from and deal with over the next several days – major surgery, bowels not in full operation yet, and narcotic withdrawal symptoms. The last thing we need is a fluid overloaded child battling with pulmonary edema when we know the standard protocol for preventing this effect in Ella. Please pray for IV Lasix – lots of it, so she is dry, dry, dry! We’ll update later with how the day continues to progress.
And as always through all of this, I am reminded:
Proverbs 3:7-8 (NLT)
Don’t be impressed with your own wisdom.
Instead, fear the Lord and turn away from evil.
Then you will have healing for your body
and strength for your bones.
UPDATE 9:30am by Tina
We feel better. It is the beginning of the week and all the docs that normally follow Ella are back in full swing this morning. They took a look at her chest xray and agree that she is fluid overloaded and plan to give her more Lasix today (and the xray was taken after two doses of Lasix). I’m hoping they will watch all of her factors more closely this time around. Plus, since they were not sharing her fluid ins/outs and her daily weight, we will be asking for that info each day. It’s not fun to babysit, but apparently we need to dig for all the details so we do not find ourselves here again.
Since Ella is fluid overloaded, she does not have tolerance for assessments and lots of touching from docs. When that happened this morning a few times, she clamps down, turns dusky and is having a tough time breathing. We’re just anxious to get some of the fluid off. But right now, they have her on a potassium drip for 2 hours to help balance out her electrolytes. As soon as that drip is finished, we will be hitting her with the Lasix for her first dose this morning.
The good news: surgery came by and said that her assessment looks good. They ordered an abdominal xray to check and make sure that none of her bowels were distended. Besides some gas trapped in there, Ella’s intestines look good. Today, we will be trying a slow drip of Nutren Jr with Fiber (10ml per hour), to see if she can tolerate it. That is a huge step for Ella, so pray that she will remain comfortable throughout the day and that her bowels will welcome the intro of food. We want lots of peeing, pooping and passing gas while remaining comfortable with the first intro of food…yeah, I know that is a lot to ask but we’re confident that it can happen!
Again, we appreciate all the prayers and support.
UPDATE 11:40am by Tina
We decided that amongst the madness, it was time to give Ella a bit of zen. Her experienced nurse had a great idea for washing her hair with all three of us doing our part, by leaning her over the edge of the bed with a basin on a table to catch the water. Mind you, she has had sponge baths but her hair had not been washed in nearly two weeks! Normally, Ella does not like baths at all. This time because she is battling the itchy symptoms, she actually was enjoying the head massage. Ahhh, a bit of Ella Spa Time.
We’re starting food finally. Let’s hope she can tolerate it.

UPDATE 1:15pm by Tina
It seemed like washing Ella’s hair made her feel good. As a matter of fact, she wanted to sit up and was getting excited. She was smiling at us, which is so good to see after several days. The only problem: her lips were blue, her heart was racing and she was desaturating even on 2 liters (it’s hard to tell in the picture below, but you can kind of see that there is blue around her mouth area). They had us increase the O2 to 3 liters.
Normally, we only see these types of symptoms when she is mad, clamps down to hold her breath and then passes out like last night which indicated a fluid issue. But this was clearly different in that she was not agitated, just excited and yet her heart and lungs could not handle the increased pressure which is a classic sign of pulmonary hypertension. The doc came in to assess her and agreed that this was a pulmonary hypertension spell. His first thought was to give her morphine to calm her and open up the pulmonary vessels. However, normally this is given if someone is agitated. You could clearly tell that she was not agitated. She was still itchy and showing signs of withdrawal, but she was playful and happy. Josh and I both do not want to sedate her more. She already acts like she’s had one too many beers, but at least she is happy and not completely drugged!
After advocating for another solution, Ella is back on nitric oxide via her nose cannulas. Until we are convinced that her sildenafil is being properly absorbed via her tummy, we feel that this is the best way to manage the pulmonary hypertension.


|
|
|
|
| |
|
|
|
|
|
|
|

So, Ella remained stable overnight. The last dose of anti-itch medicine was later yesterday evening, but we have not had to use it since. As I type this at 10:45am, she is still asleep. We may need to use Atarax or Benadryl to control the itch once she is awake. She is still taking Methadone and Ativan for withdrawal symptoms, and receiving one of those meds every 3 hours. There may be discussion of reducing the dosage, but we’ll see.
She is still on the nitric oxide to control her pulmonary hypertension and sits at 2 liters. While she is asleep, her numbers look great most of the time. We’ll see when she is awake throughout the day. It was disheartening to see her wanting to be more alert and playful yesterday and her body not able to keep up with it, thus the nitric oxide.
Once again, I’m a bit frustrated about the fluid overload situation. As of late last night around 10pm, she was still 2 liters positive for the past 4 days and her weight was 15 kilos (she was 15.1 kilos the night before). Not really any change, so I went and asked the attending if we could increase the IV Lasix dose to once every 6 hours. As of this morning, she was not positive by a lot but still positive for a 24 hour period between 100-150. It’s not a huge amount and based on her weight, they consider that inconsequential. They told me that they are only concerned if she is 300+ positive for a 24 hour period. But once again, she is still 2 liters positive for the past 4 days and Ella is fluid sensitive and does not respond like a healthy 2 year old. Being positive at all when she is already fluid overloaded is not inconsequential!!! They took a look at her chest xray from this morning and it looks unchanged from yesterday. Ya think?
When I talked with the docs, it seems that they are not getting the picture about being aggressive and really drying her out. So, I called down to CHOC Medical Records to see if I could get a print out of all the written records since admission, so I can forward it to Denver. I want her pulmonologist to see how they are treating her pulmonary hypertension and this fluid situation. I want a second opinion. Plus, he knows how different Ella responds and just how dry she needs to be for her pulmonary system to function optimally. CHOC charges 25 cents per page to fax it over to Denver (ridiculous), but I’m going to take on the expense because I need a pulmonology expert to weigh in. Overall, CHOC has been great but they do not know Ella and continue to treat her with the same protocol as other patients AND they do not have any pulmonology experts (Denver has 18 – it is a speciality for them). All we did yesterday was give her enough Lasix to maintain her in the same place. They are not being aggressive enough and treating her pulmonary status in a way that I am comfortable with – so – it’s time to get Denver more involved.
On a positive note, Ella seemed to tolerate her food at 10ml per hour just fine without any discomfort. So, surgery would like to increase her rate to 20ml today and try it. However, they are waiting to see if Ella will stool. Her last bowel movement was Sunday afternoon. She has been taking her home regiment of Miralax for the past few days. So if she doesn’t stool on her own soon, they will look to give a suppository later today and want to see another stool before letting her increase on her rate of food.
In the meantime, I’m advocating and ruffling feathers in the PICU. I guess it’s my role in life. Sigh…
Psalm 68:19
Praise be to the Lord, to God our Savior,
who daily bears our burdens.
|
|
|
|
| |
|
|
|
|
|
|
|

Sorry for the late post – it is literally the first break I’ve had all day. So much has happened since yesterday’s post…where do I start?
Yesterday morning at rounds, I expressed that I was going to involve Denver in our discussion. Ella’s lungs are too wet and we need to dry her out. We did not make much progress in the 24 hours prior and I wanted them to get more aggressive. After I talked with Ella’s pulmonologist (who is amazing), I had the PICU attending call and speak to him as well. After their discussion, the nitric oxide machine was calibrated upward to 10 parts per million and Ella received a dose of Bumex, in addition to the IV doses of Lasix. It made me feel better to know that our pulmonologist was giving his opinion and letting the PICU doctors know that Ella needs to be more dry than an average kid.
Surgery came by to visit. Since Ella had tolerated 10ml per hour, they wanted her to stool first, but then increase the rate to 20ml per hour. While the surgeon was standing there, Ella had a melt down moment and passed out within several seconds. The surgeon was so surprised – it completely took her off guard. She affirmed to us that is not something she has ever seen happen before that quickly. Again with fluid on Ella’s lungs, this can happen often. While Ella was clamping down during this episode, she also pooped – right in front of the surgeon! So once that happened, the surgeon wrote an order to increase her feeds to 20ml per hour.
Around 2:15pm, the PICU docs also considered giving Ella another diuretic to help make the Lasix more effective. It is called Metalazone and it is a thiazide diuretic that works the other side of the kidney. It is only given in an oral form via her g-tube, so we were not sure how much would be absorbed, but figured we would give it a try. Within 10 minutes of giving the medicine, she was writhing in pain. We saw this the other day when we tried to give her Methadone in the oral format. So we stopped the food pump, vented her to let any gas out, and tried to let it back in but she fussed. The return from the g-tube was yellow in color (not too concerning, just gastric juices). So, we left it in a cup off to the side and thought we would give her a break and try later. Since we thought the medicine was likely irritating her belly, we never put it back in. After a 30 minute break, we turned the food pump back on. Two hours later, Ella complained again. This time, we had not given any medicine through her g-tube. We vented and Ella returned a bunch of food and gas. Both times, she returned about 40ccs from her belly. If her food pump was at a rate of 20ccs per hour, then this means that her tummy is not emptying real well.
They consulted surgery at 4:30pm and they advised to turn off the feeds and let her rest. Two hours later, we vented and got about 30ccs of green bile returned. Green is not the color that we want to see. This was a bit concerning. When we weighed her last night, she was 14.3 kilos, tonight she was 14.4 kilos. She was 15 kilos the night before. We are happy with the weight loss and could tell that she was saturating better today.
Last night, she did fine but woke up at 3am, crying. She had a spell where she dipped down into the 30s and passed out within seconds. The nurse gave her some meds and she settled back down. At 6am, they came to take a chest xray (turned out that her lungs looked much better than yesterday). The technician was not real gentle and she woke up Ella. This made her mad and she had another pass out moment. When she recovered from that, she started crying hard again like she was in pain. She was holding her breath and desaturating – she passed out again. All of a sudden, you could hear gas and runny poop. This happened again later this afternoon, so we gave her a suppository to help with stooling (on top of her Miralax). But again this evening we had another pass out moment right as she was pooping, so we have resolved that she must be having some pain associated with passing gas and stooling.
Surgery decided to hold off on food again today and let her rest. With the pass out spells and so many other factors, they wanted to let her rest and will reassess tomorrow. They plan on taking another abdominal xray tomorrow to make sure that her bowels are not distended again and that there is nothing wrong with her physiology since the surgery. If everything looks okay (similar to her last xray), then it is likely just motility issues.
They did give her another echo yesterday because she was having these spells, but they have not told us the final results. I’m hoping to hear tomorrow. In the meantime, they decided to increase the nitric oxide to 20 parts per million this morning via nasal cannula. Her color has not looked great all day, sometimes better than others. It’s hard to tell from the photo, but even her eyes are purple and look bruised (they kind of match her binky).
Her potassium has been running low, so between doses of Lasix, they’ve had to give her a slow drip of potassium. In order to try and help that process, they decided to switch her diuretic to aldactazide. The docs in Denver have given Ella aldactazide before since it is a potassium sparing diuretic.
She does seem very touchy and gets agitated very easily. We’re having to keep her on the doses of withdrawal meds every 3 hours plus Atarax and Benadryl for itching. Yesterday, we had to give her a dose of morphine to keep her calm on top of these meds. Today, we had to give her morphine twice. Sigh…between all her regular medicines, plus the withdrawal meds, she is one drugged child: sildenafil, reglan, zantac, miralax, aldactazide. She gets 2 shots of Lovenox every day instead of aspirin and plavix to help with anti-coagulation. Then, Ativan and Methadone for withdrawal. Also, Atarax and Benadryl for itching. Then, morphine to keep her calm. And of course, some of these meds can’t be good for motility either.
There was discussion this afternoon about giving Ella a blood transfusion. The cardiologist wondered if it had anything to do with Ella’s pass out moments. Your hemotocrit is the proportion of blood volume that makes up red blood cells. Red blood cells are the carriers of oxygen in the blood. Since Ella’s system has been under strain and her hematocrit is lower, he thought this might help her. Upon admission, her hemotocrit was 13.7. For the past several days, it has stayed around 8.5. Typically, they only strongly recommend a blood transfusion if it is below 8. Considering all the strain that her body is under along with her history, a blood transfusion might help her and certainly wouldn’t harm her aside from the inherent risks of a blood transfusion. Ella had blood transfusions in the NICU several times, but her levels were at a critical point where she needed them. Since we have had plenty of pass out spells with Ella and we have never given a blood transfusion, we didn’t feel led to take that step at this time.
We’ll see what the team thinks tomorrow about her overall fluid status, pulmonary hypertension, pass out spells, and the general motility of her guts since surgery. I did chuckle when the attending came over to us after rounds and asked how long we were planning to stay. He knows that we are not from the area and you could tell that there was concern. He wanted to make sure that we were prepared that this still might take a while. He told us that his best guess (if she stays on the same track) is 2 weeks. Yikes…
Tonight @ 10:30pm, Ella seems unsettled even though she has had Morphine, Benadryl and Ativan in the last two hours. I have a feeling that tonight might not be so restful. Actually it now 11:00pm and I just had to take a break from writing this to console her – but she was not consolable – so they just gave her another dose of Morphine. My heart is heavy – I hate using all these drugs. I miss seeing my daughter. This withdrawal from the narcotics has been the worst. We’ve been at it for a week with no end in sight. Please pray for the Lord to miraculously resolve Ella’s withdrawal symptoms.
2 Timothy 2:13 (NLT)
If we are unfaithful,
he remains faithful,
for he cannot deny who he is.
|
|
|
|
| |
|
|
|
Posted ( jooosh) in All Posts on April-22-2010 |
|
|

Well, Tina was right in her prediction on the previous post. Ella decided to wake up around 4am this morning with spells of agitation and fussiness. Benadryl and morphine were given, but she didn’t settle back in until 5:30am.
Around 6am they came by for an x-ray. A chest x-ray was ordered and we thought the surgery team wanted an abdominal xray too. They did, but the order wasn’t in the system when the tech came around. Bummer because it would have been nice to knock them both out at once.
Ella continued to be fussy throughout the morning. When Ella is in this state in can be incredibly exhausting to deal with. On top of seeing your kid not feel well, it can be extra challenging because Ella can’t tell us exactly what she wants. Most of the time, we guess correctly based on her body language, but there are times when you try everything and nothing seems to console her.
Tina has been by Ella’s side almost the entire time we’ve been here. As her mother, I know she wants to make sure Ella’s taken care of, and she’s very protective of our sweet child. It’s hard to convince Tina to break away, and she’s really only been away from the hospital couple times. I try my best to push her out of this place, but Ella’s current instability keeps her here. Today Tina took a real break though. She had lunch with a dear friend that we’ve known for many years. I’m so glad she was able to escape. She was gone for a good 4 hours. I’m hoping I can talk her into getting away more often on a regular basis.
While Tina was gone, Ella maintained her agitated fussy mood, that is, until the docs did rounds. All of a sudden it was like a switch: Ella was happy and a LOT more like herself. Sitting up, smiling, engaging us, reacting to us…just totally typical Ella behaviors. She is still on a heavy dose of meds, which makes it look like she’s had a few beers, but other than that, she’s just being more like herself. She had a honeymoon period like this briefly a few days ago, but not really since. But this time, she maintained her mood for a couple hours, right up until Tina came back from lunch. For whatever reason, Ella became agitated again, and had a major episode (desaturating and passing out). This fussiness continued all the way up until dinner, and then…she was happy again and continues to be so even as I write this. We’re really not sure why she is having these kind of swings, but at least we’re seeing some of our true kiddo break through. I hope and pray this trend continues because we’ve really missed our sweet child.
When the docs did rounds this morning a couple changes were made. They wanted to discontinue all of her PO meds, even her sildenafil because they were convinced they were not being absorbed enough to make a difference. I convinced the attending to at least keep the slidenafil even if it’s only being absorbed a little. It’s such a key component to helping Ella’s pulmonary hypertension that even if she’s only getting some on top of the NO (nitric oxide), I think it’s better than not giving it. He agreed but also confirmed he was doing it so we couldn’t point to him DCing it as a potential sticking point later. I smiled and said, “I definitely understand that”. =)
The other reason for them wanting to discontinue the PO meds was due to what they saw on the abdominal x-ray. It looked as though Ella had another significant distended loop in her intestine. Oye…this was a bummer to see. The attending confirmed that it might not be anything too concerning, but they want to keep giving her bowels a rest and see if it resolves. We did have a doc from the surgical team come around later, and he confirmed that it shouldn’t be anything to worry about. In fact, he thought it was just her colon and not small intestine. (Whew) We’ll confirm for sure with Ella’s primary surgeon, but if all looks good with this and the rest of her gut, we’ll probably try food again tomorrow.
The docs also saw that her chest x-ray today was more “wet” than the one yesterday. So even though she is getting a strong dose of Lasix every 6 hours, that’s still not enough to diurese her. They hit her with another dose of Bumex this morning and she peed out a 418cc diaper (normally Lasix produces 100-178 per diaper)! This has to be surprising to them considering they were hesitant to give Lasix every 6 hours instead of every 8 hours. We tried to tell them, but I think our pulmonologist in Denver affirmed this too. Either way, Ella just confirmed what we’ve said from the beginning. When Ella means dry, she REALLY means dry. Maybe we should get her a tee-shirt to wear with this on it:
The other suggestions that were made on rounds were to get a Nurse Practitioner from pain management involved as well as an individual that specializes in Chinese Medicine. For pain management, we want other thoughts on which meds to be giving to help with withdrawal. It seems like we are having to give so many drugs to keep her comfortable. Plus, she is still itchy. So, we’re hoping to get some insight from her. Also, the thought was to look into using acupuncture to help Ella. We’re excited to explore this area of medicine as we’ve never been presented the option before. Very cool that CHOC has it available here.
We’re so pleasantly surprised to Ella even slightly return to herself this evening. It was shocking because it came from out of now where and moments earlier she seemed so agitated. But we know that He can perform miracles and that all of you are diligently praying for her. We’re hoping that this was not a fluke – it would be great to think that Ella is actually turning a corner. The test will be in the hours to come.
Thank you all for your continued thoughts and prayer support. It means so much during this time.
1 Thessalonians 5:16-18 (NLT)
Always be joyful. Never stop praying. Be thankful in all circumstances, for this is God’s will for you who belong to Christ Jesus.

|
|
|
|
| |
|
|
|
|
|
|
|
The doctors don’t have an explanation…but Ella started acting like herself last night at 7:30pm. She was in a great mood for a few hours, went to sleep. She woke up at 4am when the nurse changed her diaper. After 15-20 minutes, she cried herself back to sleep. She has been in an amazing mood all day, kicking her legs and smiling. Heck, she’s even been sitting up in the hospital crib, getting tangled in all her wires!
They gave more Bumex last night and she weighed in at 14 kilos, so she is still losing fluid. Her chest xray looked improved this morning. They continue to give Lasix every 6 hours and supplement with Bumex when she is positive on her fluids. Tonight, she is due for Lasix at 8pm and Bumex at 10:30pm, based on her ins/outs. She sits at 2 liters of oxygen and on 20 parts per million of nitric oxide via the nose cannulas. They are realizing how touchy her pulmonary status can be and don’t want to wean or make any changes until they have resolved some of her other issues and know that her Sildenafil is being absorbed via her tummy.
The only time she has gotten annoyed today is when she wants to drink water. You can hardly blame her – she’s so thristy from being so dried out with the diuretics.
There are so many things to make forward progress with on this child, so it is a matter of choosing one area to focus on, going slow and getting some victories. For today, they decided to try food. This time they wanted to go even slower, 5ml per hour of Nutren Jr with Fiber. Ella still had a challenge with it initially today because she gets too much air trapped in her belly when using a continous drip of food and she is still not passing gas like she does normally. So when that air gets trapped, it causes her gas pains. Instead, we talked them into letting us drip it over 30 minutes on the pump then venting for 30 minutes. Each time we vent, we usually get gas out. It has worked fine throughout today and she has been tolerating the food fine. She has been watching her videos and having a great day. We’ll see what happens over the next 24 hours. There is still concern that it could be a cumulative effect and that by the time more food gets in her, she may have slow motility or slow gastric emptying. Either way, time will tell.
Tomorrow, there is discussion of weaning her off of the withdrawal meds: Methadone and Ativan. They want to go very slowly over about a 2-3 week timeframe. They will continue to give one or the other every 3 hours, but slowly wean the dose of med.
They discontinued Benadryl yesterday and we have not given any Atarax today. She has not shown one sign of being itchy. Wow.
We have not given any Morphine because she has not shown any signs of being agitated. Wow.
She is happy and smiling. You would never even know that she was checked out the past two weeks. Wow.
We realize that there still may be bumps in the road in the coming days, but this was a true testament to prayer. Again, the doctors have no explanation for the sudden turn. We thank all of you for the prayer support and are so thankful to see our daughter smiling and feeling good today. Whether the days ahead are darker, it was a clear indication to us that He is in the midst of the chaos.
1 John 5:14-15 (NIV)
This is the confidence we have in approaching God: that if we ask anything according to his will, he hears us. And if we know that he hears us—whatever we ask—we know that we have what we asked of him.

|
|
|
|
| |
|
|
|
|
|
|
|
Ella’s day was a bit more rough – yesterday was definitely the honeymoon to get us through the coming days and provide hope.
The docs wanted to make too many changes and Ella rebelled. First, the pain management team came up with a plan to wean the Ativan from 1.5mg to 1.2mg. After a couple of hours, she started to have withdrawal symptoms. She was more shaky and just seemed agitated. Fortunately, no itch but she was clearly uncomfortable in her own skin. We ended up giving the missing amount of Ativan plus a little extra just to settle her down. The plan was to wean Methadone tomorrow. At this point, I’m not sure if they will still try or not. Throughout the day, I did notice that if the nurse was not regimented about giving one of the withdrawal meds on time, Ella let us know.
Along with Ativan, they increased her food from 5ml to 10ml per hour. We tried giving 10ml over 30 minutes and venting/resting for 30 minutes on and off. A few times though, we got clear tummy pain. When we would vent, we would get return that was a bit green in color and TONS of air. Sometimes when venting we could connect her manually with the syringe and nothing seemed to happen. But if we drew back on the syringe, we got lots and lots of air. Also, we would get anywhere from 20-40ccs in the syringe. This meant that she was not emptying as quickly. This has been our concern all along: slow gastric emptying and slow motility. Since she seemed to be having tummy pain and we wanted to see if it was her tummy versus lower intestinal pain, we got approval for a dose of Maalox. Thankfully that did the trick by neutralizing the acids in her tummy and within 10 minutes, she was calm.

Later in the day, I convinced the nurse to give her a rest from the feeds. We drew back in the syringe and she had 40ccs of formula in her belly. When you’re only feeding at a rate of 10ccs per hour, it was clear that she was not emptying real well. However once we vented all the air out, we could bolus the 40ccs right back into her via gravity, and she tolerated it fine. So we decided to give her a 2 hour break and I convinced the nurse that this was an example of how Ella tolerates bolus feed schedules better. We waited 2 hours, gave 20ccs of formula and didn’t bother her again for 2 hours. The good news: I don’t think that the formula is giving her any problems or discomfort. Plus, she had another poop tonight. This means that overall things are working. We just need to be patient on moving forward with the volumes and make sure that the gastric emptying and motility is working.
Another symptom today: tons of mucoids. Wow. Just lots of really thick secretions. Since she was so thirsty, we were giving water by mouth which was helping to break them up. But then she would cough, retch and soil the bed. We had to change it a few times. Thankfully, Josh and I were both here when these happened and Josh was able to grab Ella and lean her over so the mucoid would come out of her mouth onto the bed instead of her re-swallowing them. Along with mucoids, she was retching a lot. Oh, I wish that retching was not a daily activity. Just as we’ve noted before, it is definitely associated with her feeding via g-tube. When we were not dealing with food the past 2 weeks, we had no retching. Somehow food must be refluxing or just the pressure of her belly having something in it, even just the smallest amount is causing the retching.
The docs decided that Ella was not outputting enough urine, so they’ve increased her Lasix to 20mg per kilo every 6 hours. Plus, they are still giving Bumex, here and there. She had one dose of Bumex this morning and a chest xray is scheduled for the morning to check her fluid status. Right now, she is even on ins/outs for the day. I know that this will be another area where we need to try and wean to get back to a reasonable dose of diuretics for our trip home. We are able to dry her out to this extreme in a hospital setting where they draw labs and check her electrolytes all the time. But once we are back to a home routine, we cannot give this amount of diuretic. I’m bummed that we’ve had to use Bumex this hospitalization (we went 14 months without using it at all). It will just be interesting to see how the diuretics end up working out this round.
Her central line has been in her femoral artery (her thigh) since her day of surgery, 2 weeks ago. There is a decent amount of risk for infection as the days continue. And we have several days of hospitalization ahead of us where we need to be able to give IV meds, IV drips and do blood draws. So the plan is to switch to a PICC line on Monday (peripherally inserted central catheter). A PICC is inserted in a peripheral vein and then advanced through increasingly larger veins, toward the heart until the tip rests in the distal superior vena cava or cavoatrial junction. The last time she had a PICC line was the NICU. Hopefully, they can get it on the first try.
One cool thing: my brother and sister-in-law know a physical therapist that works here at CHOC. I ran into her today and asked for a favor. I wanted to see if we could get one of those chairs to sit in Ella’s crib. I figured it would help drain secretions and help with gastric emptying. Plus since Ella still acts like she has had a few beers, it would allow her to sit up and not work quite so hard. Apparently, the rehab/physical therapy department does not normally come and leave their tools in the PICU because they end up getting lost. But she made an exception for Ella due to the connection with my family! It will be a nice tool to use over the coming days.
In between the fussy times of discomfort and sedated moments from withdrawal meds, we did see glimpses of Ella. She would get excited, smile and play. Although the day was a bit rough, we still made a tiny amount of forward progress with feeds. We’ll see what tomorrow brings.
|
|
|
|
| |
|
|
|
|
|
|
|

Last night was rough again for Ella. We only had a few hours of sleep.
She had a chest xray this morning which looked good and so they made a few changes today. First off, the respiratory therapists have been weaning oxygen during the night shift while I was asleep and not telling me! It was nice to see her at .5 liters this morning (her baseline while at sea level). However by noon, she was not saturating well. They weaned too fast so they had to turn her up. Right now, she is on 1 liter and seems to be stable. The doctors ordered to turn down the nitric oxide to 10 parts per million. Also, they decided to wean the methadone slightly.
Ella had moments of feeling fine, especially right after her withdrawal meds (like above sitting in her chair). She would get excited and happy. But then at other times, she would get very fussy and agitated, sometimes jittery and itchy. In between, she went through times of the day where she just did not want to be bothered – not even from mom or dad.
Another challenge the past few days: she is so thirsty from being dried out. She wants to take water by mouth, but it needs to be limited since they need to limit her intake. That is tough to not give her water when you know that she is so thirsty. When we have to stop giving the water throughout the day, she would get very agitated. It’s been challenging.
We were able to make some progress with food. The docs were interested in increasing her volume and I requested to stay at the same amount since we had some challenges yesterday. We stayed at 10ml per hour today, but I would bolus 20ml and let her rest for 2 hours. She handled the food and the volume fine. We gave Maalox once last night at 3am and once at 3pm to help relieve tummy pains. Otherwise, her tummy seemed to empty faster today.
We’ll see what changes come about tomorrow as we start another week. Thanks again for the thoughts and prayers.
Psalm 62:8 (NIV)
Trust in him at all times, O people;
pour out your hearts to him,
for God is our refuge.
|
|
|
|
|
|