| |
|
|
|
|
|
|
|

Remember on yesterday’s post how I mentioned that we were seeing Ella go in the wrong direction. I warned the resident during the day shift and they just wanted to “watch and see”. Later last night, it just kept getting worse. Ella had two episodes where she got upset and her saturations dropped into the 30s and she passed out on me – – twice! When this happened, we increased her to 2.5 liters and it still took a good amount of time for her to come back up. This pushed Josh and I to put on our armor and start war with the night resident. Although this particular resident had not been following her all the time, we pled our case: based on everything we know about Ella, she has to be fluid overloaded.
Then, we started asking for the facts since we’re not even convinced that she was dried out enough after surgery. How fluid positive is she for the past few days since you halted IV Lasix? We found out that she had been fluid positive 2 liters! That is the same amount as the day after surgery. Then, I asked about her weight which is another indicator. Remember when I mentioned that Ella lost weight? Well, she was 13.6 kilos three nights ago (29.92 pounds). Tonight, she was 15.1 kilos (33 pounds). She is on IV drips for nourishment, so there is no way that a 2 year old would gain 3 pounds in 3 days!
This is so frustrating. We feel like we are back at square one and that they are not listening to us about her fluid sensitivity. We had the same frustration initially in Denver until we were there for nearly 10 weeks! We are only at a week and a half, but this is painful.
After we discussed with the night resident, we negotiated one dose of Lasix at 8:30pm to see what would happen. Ella responded within the hour and peed out 178ccs. Next, we asked about another dose in 6 hours at 2:30am. At first, the resident only wanted to give a half of a dose of Lasix. That was not going to fly. Josh had already left for the night, so I put on my armor and had another discussion with the resident shy of midnight. I was able to negotiate another full dose scheduled at 2:30am. Before the nurse administered it, we changed a diaper with 95ccs. The dose of Lasix at 2:30am produced 378ccs of pee! She also had a chest xray this morning at 5:30am.
We will continue the battle with the day shift. Please pray that they will begin to listen to us about Ella’s physiology and her needs. She is not text book and they need to consider her specific needs, not the standard care of protocol. Our baby girl has so many things to recover from and deal with over the next several days – major surgery, bowels not in full operation yet, and narcotic withdrawal symptoms. The last thing we need is a fluid overloaded child battling with pulmonary edema when we know the standard protocol for preventing this effect in Ella. Please pray for IV Lasix – lots of it, so she is dry, dry, dry! We’ll update later with how the day continues to progress.
And as always through all of this, I am reminded:
Proverbs 3:7-8 (NLT)
Don’t be impressed with your own wisdom.
Instead, fear the Lord and turn away from evil.
Then you will have healing for your body
and strength for your bones.
UPDATE 9:30am by Tina
We feel better. It is the beginning of the week and all the docs that normally follow Ella are back in full swing this morning. They took a look at her chest xray and agree that she is fluid overloaded and plan to give her more Lasix today (and the xray was taken after two doses of Lasix). I’m hoping they will watch all of her factors more closely this time around. Plus, since they were not sharing her fluid ins/outs and her daily weight, we will be asking for that info each day. It’s not fun to babysit, but apparently we need to dig for all the details so we do not find ourselves here again.
Since Ella is fluid overloaded, she does not have tolerance for assessments and lots of touching from docs. When that happened this morning a few times, she clamps down, turns dusky and is having a tough time breathing. We’re just anxious to get some of the fluid off. But right now, they have her on a potassium drip for 2 hours to help balance out her electrolytes. As soon as that drip is finished, we will be hitting her with the Lasix for her first dose this morning.
The good news: surgery came by and said that her assessment looks good. They ordered an abdominal xray to check and make sure that none of her bowels were distended. Besides some gas trapped in there, Ella’s intestines look good. Today, we will be trying a slow drip of Nutren Jr with Fiber (10ml per hour), to see if she can tolerate it. That is a huge step for Ella, so pray that she will remain comfortable throughout the day and that her bowels will welcome the intro of food. We want lots of peeing, pooping and passing gas while remaining comfortable with the first intro of food…yeah, I know that is a lot to ask but we’re confident that it can happen!
Again, we appreciate all the prayers and support.
UPDATE 11:40am by Tina
We decided that amongst the madness, it was time to give Ella a bit of zen. Her experienced nurse had a great idea for washing her hair with all three of us doing our part, by leaning her over the edge of the bed with a basin on a table to catch the water. Mind you, she has had sponge baths but her hair had not been washed in nearly two weeks! Normally, Ella does not like baths at all. This time because she is battling the itchy symptoms, she actually was enjoying the head massage. Ahhh, a bit of Ella Spa Time.
We’re starting food finally. Let’s hope she can tolerate it.

UPDATE 1:15pm by Tina
It seemed like washing Ella’s hair made her feel good. As a matter of fact, she wanted to sit up and was getting excited. She was smiling at us, which is so good to see after several days. The only problem: her lips were blue, her heart was racing and she was desaturating even on 2 liters (it’s hard to tell in the picture below, but you can kind of see that there is blue around her mouth area). They had us increase the O2 to 3 liters.
Normally, we only see these types of symptoms when she is mad, clamps down to hold her breath and then passes out like last night which indicated a fluid issue. But this was clearly different in that she was not agitated, just excited and yet her heart and lungs could not handle the increased pressure which is a classic sign of pulmonary hypertension. The doc came in to assess her and agreed that this was a pulmonary hypertension spell. His first thought was to give her morphine to calm her and open up the pulmonary vessels. However, normally this is given if someone is agitated. You could clearly tell that she was not agitated. She was still itchy and showing signs of withdrawal, but she was playful and happy. Josh and I both do not want to sedate her more. She already acts like she’s had one too many beers, but at least she is happy and not completely drugged!
After advocating for another solution, Ella is back on nitric oxide via her nose cannulas. Until we are convinced that her sildenafil is being properly absorbed via her tummy, we feel that this is the best way to manage the pulmonary hypertension.


|
|
|
|
| |
|
|
|
Posted ( jooosh) in All Posts on April-18-2010 |
|
|

We’ll give a quick update, but with all the not so fun times we’re experiencing now, we figured a photo break escape for you Ella fans would be good. But first…
Ella’s hanging in there, but the parents are exhausted. Her withdrawal symptoms have lessened a little bit, but she still very spacey and itchy. She slept through the night and had a good morning. She was awake for about 2 hours last night and then has been for most of today although she is still sedated. We have tried not to give any additional doses of morphine and have been able to avoid it thus far. One surprise today: she actually tried to sit up in the bed even though she didn’t have the balance or strength to sit on her own! That is her fighting spirit trying to work through the withdrawal meds!

Surgery came by to take a look at her: they still wanted to hold off on food. Once we heard the news, the PICU team thought it might be good to try her withdrawal meds via her g-tube versus IV. A small change, but one in the right direction (since we will have to wean the withdrawal meds at home too). However, they gave methadone via g-tube and within 10 minutes, she was writhing in pain. Apparently, her tummy really hurt. We vented her belly as much as possible and after 15 minutes, she was content again. So, they had to order the withdrawal medicines via IV again.
Ella’s hand looked puffy at the IV site and although it was still flushing, it had been active for 10 days. So, we were able to take it off today to give her hand a break. We checked the central line to make sure that we could still draw labs and it appeared that there were clots in the line. They ordered a TPA (tissue plasminogen activator) to clean up the catheter and eliminate clots. Fortunately, it worked and they are now able to draw off of two more lumens. Thank goodness!
We had asked the docs as well if they were sure that she’s experiencing withdrawal symptoms and not something else. With all the symptoms Ella is presenting though, we’re confident that we’re treating withdrawal. They have a Finnigan scale where they score her each day to see where she ranks on the scale. Ella is presenting most of the signs of true narcotic withdrawal. It’s so difficult seeing your kiddo deal with this when just a few weeks ago we were all enjoying our time together.

One more concern: this afternoon, she seems like her respiratory rate is higher, heart rate a bit higher and saturations not as good. Knowing Ella, it might be fluid related. She has been positive for urine output the past few days. Maybe the net effect is accumulating and we’re seeing signs of fluid retention. On a similar note, they increased her dosage of sildenafil because the echo showed that it was not all being absorbed through her g-tube. Maybe her diuretic is doing the same thing? If she continues this way overnight, we’ll likely be requesting a chest xray in the morning, just to eliminate that possibility.
Please continue to pray for the Bun’s healing and forward progress.
Below are some pictures of our trip since we hit California back in March. Enjoy…

Lovin’ on Grandma West
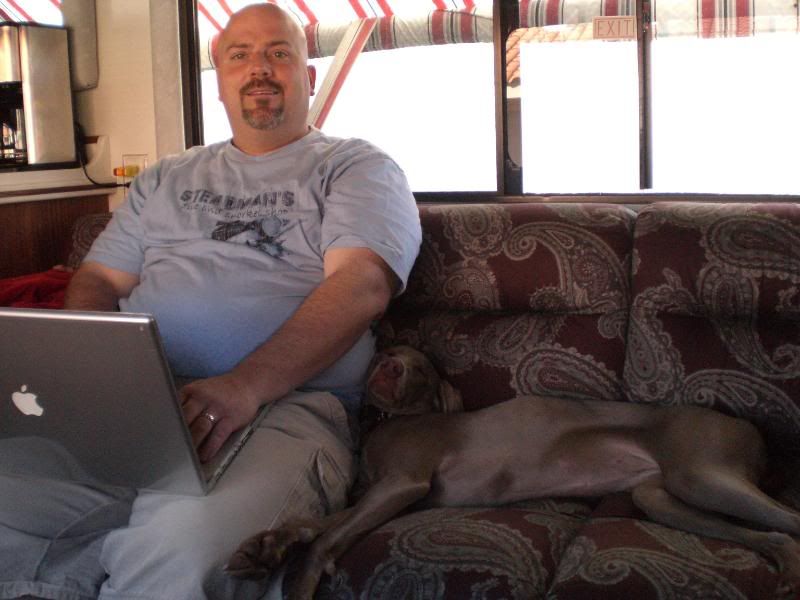
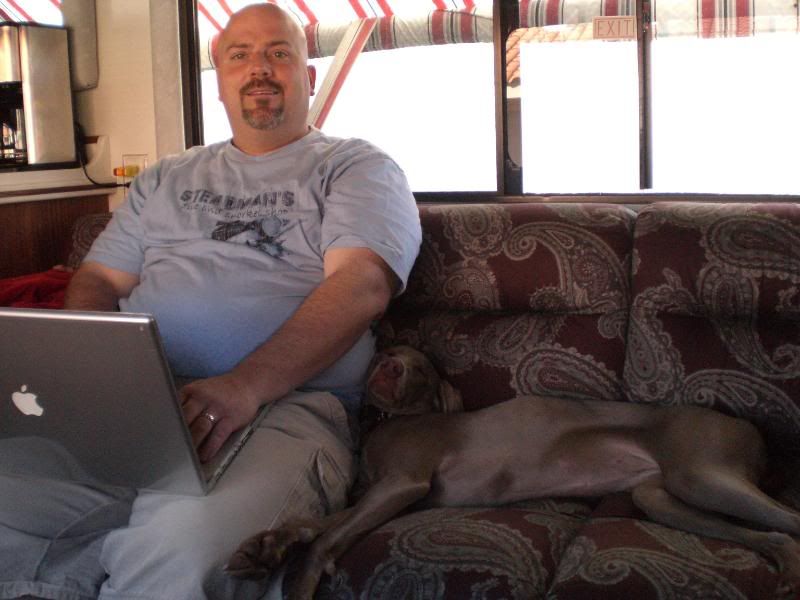
Ella’s dad and his asistant
Contortionist Pooch

Ahhhh…the Pacific Coast

Waiting in line

Nothing like a beautiful sunset to inspire black water dumping

The Rig

Rockstars!

Unnecessary extreme closeup self portrait

“Yay! Dad’s dumping the black water”

Don’t ask, Don’t tell

Even the pooch enjoys a good sunset

I’m givin’ it all I can captain…I think she’s gonna blow!!!

Ummm…semi-fresh water spray?

I have me some mad dumping hose cleaning skillz (ummm…are you wearing flip flops???)

How cute can you get?

Even cuter!

EVEN CUTER!

Standin’ up baby

Yeah…pretty stinkin’ cute!

Out in the stroller

A pooch and her Kong

Ella, “Can I have the Kong?”

Lola, “Yeah…no…I don’t think so!”

Pooch refill

Restin’ on poppa

Diva dog pose

PCH in Laguna Beach

The beach in Laguna

Face to face with cousins for the first time!

Richard and Megan

Richard and Megan again

The whole crew

What’s goin’ on outside?
Excuse me sir, do you have tickets to the gun show?

Megan and Aunt Tina

A sleeping Lo

Cousins Claire and Ryan!

Sleepin’ Bun

Great Grandma and the pooch

Ella’s Great Grandparents

Silly Bun

Nap time

The Rig in front of the Great Grandparent’s house

O2 Pickup at Apria

Pooch walkin’ at Doheney State Beach

The parking spot

Lola enjoying the view…and…well…enjoying being a dog

Silly Dad

Cute Patoot

The smiles melt your heart

The melting continues

More cuteness

Just darling

Woah!!!

What’s this!!!!

Look Ma…no cannulas!!

West Family Self Portrait
|
|
|
|
| |
|
|
|
Posted ( jooosh) in All Posts on April-17-2010 |
|
|

Last night was hard. The medicines to help treat the narcotic withdrawal symptoms plus the itchy symptoms were being administered once every 3 hours. It seems like Ella has already built up a tolerance because at 4am, she could not stop itching and wiggling around the bed. Unfortunately, they could not give her anything to help with the relief. She was wiggling and upset till 6am, when they gave her more meds.
This behavior was shared with the doctors. With this in mind they decided to give a half dose of morphine in between the other meds to possibly help with the withdrawal symptoms. The nurse gave the first dose this morning, and unfortunately, it did nothing for her. One of the docs came by and saw Ella having another episode in the afternoon. They decided to up the dose of morphine hoping it would help. We haven’t use it yet, but there’s a good chance we will have to later.
Tina and I are upset that they have to pump Ella so full of these other meds just to help her recover from the withdrawal symptoms. Even once the symptoms calm down, we’ll have to wean her off these other meds. Granted, we won’t need to be in the hospital to do this, but it could still take up to 6 weeks to titrate the methdone and ativan! Uhhhh…such a bummer.
Ella had a echo done yesterday, but we didn’t hear the definitive results until today. It looked the same as when she was on the NO (nitric oxide) showing mild pulmonary hypertension. This means that the current dose of sildenafil isn’t working like it normally does for her. Our guess is that it’s being absorbed in the stomach but not in the small intestine, minimizing the impact. The docs ordered an increased dose for now until her small intestines are back in line. Hopefully this is all it takes to get her pulmonary hypertension back under control.
Tina also reminded the docs during rounds that Ella was on a regular dose of Miralax at home. They admitted forgetting this fact and wrote an order for her to be put back on it. As of this time, there’s no set date on when we get to start feeding her. The surgery team came by and confirmed that we should still hold off on the food for now. The head surgeon listened to her bowels and, just by the sound, was able to tell that she’s still too distended and not ready. He also affirmed that all the other meds we’re giving to minimize Ella’s withdrawal symptoms will slow down her motility as well. So for now the kiddo is on a steady diet of TPN and lipids via her IV.
With all the complications still in the way, it doens’t look like we’ll be moving out of the PICU for a bit. I guess we’ll consider that a silver lining.
Thanks to all of you who have brought us dinner, sent cards, delivered gift baskets, and visited. The greatest blessing of being in California during this time is the fact that family and friends can support us with their physical presence. Your amazing love, support, and prayers keeps us sane. We also appreciate all the virtual love and support from our friends and family across the country. Thanks for being here with us!
Please continue to pray for our sweet girl…that her withdrawal symptoms will subside, her body will heal, and the Lords work will be done through the circumstances he’s having us go through.
Thank you Lord for bringing us here and for carrying us through this incredibly challenging time. We know you’re in control, and we trust in you, but it is hard to see your child go through this. We know you, Father, can relate. Jesus, we ask that you comfort our child and reduce her withdrawal symtoms. Heal her body, and make her whole again. We praise you Lord for the precious child you’ve blessed us with. Thank you for her. We love her so much. Amen
|
|
|
|
| |
|
|
|
Posted ( jooosh) in All Posts on April-16-2010 |
|
|

At the moment the kiddo is resting. She’s been doing a lot of this the last day. AS a matter of fact, since last night around 10pm and it is 5:30pm today and she has not stopped sleeping. I think it’s a combo of her body wanting to rest, plus the bevy of meds that are making her sleepy. I’ll tell you though, I’m happy to have her sleeping considering the alternative. Seeing your kiddo go through narcotic withdrawal symptoms is one of the hardest things I’ve ever had to watch.
She shakes and babbles and doesn’t act like herself plus she is so itchy. It’s really heartbreaking and scary at the same time. There’s also no way to know for sure how much longer it will last either. I mean, the symptoms will go away eventually, but it could last even another week! She has some moments of lucidity when the methadone and ativan hit her just right, but it’s not all the time yet. So keep sleeping sweet girl.
On a more positive note, Ella’s bowels are moving along. She had her first poop last night (yay) which is always a big deal after surgery, let alone bowel surgery. They docs are pushing to switch all meds to PO (by mouth/g-tube for Ella), and so far Ella is processing them in her tummy just fine.
We had an unofficial confirmation of this when she had her echo done. The docs had the NO (nitric oxide) stopped and checked her heart to see if the sildenafil was now working instead for her pulmonary hypertension. Peeking over the tech’s shoulder, he confirmed that her echo looked good compared to the previous one. Yay for Ella’s body moving forward! If Ella keeps this track, the next steps will be introducing food back into her system. The rumor is that a very slow drip of food into her g-tube might happen as quickly as tomorrow.
One small bummer is with all the positive steps forward, there’s a good chance they’ll move us out of the PICU. For Ella it’s a good thing, but for her parents it’s going to present some challenges. The regular rooms are shared, which isn’t an issue, unless some kiddo comes in with some major cold putting Ella at risk. They’re not supposed to put kids like this in a room with Ella, but they do. Plus, no couch/bed to sleep on, so we’ll* probably be catching our winks in a chair. Here’s hoping that somehow we can be discharged right from the PICU, but I have a feeling that won’t happen.

Ella’s Grandma West came for a visit yesterday evening. She made Ella this beautiful blanket and matching cover for her frog pillow. Grandma West got to see Ella during one of her more lucid moments, which was enjoyable for both.
Please continue to pray for our sweet girl as she progresses forward. The support that you all have given to us over the last week has meant so much. It really carries us through these times.
P.S. Lola the pooch is still sick. Hoping her antibiotics kick in soon.
*By “we’ll” I mean my saint of a wife who has been staying next to Ella every night so far. Sleeping on a chair stinks so I may be pushing her to sleep in the rig a couple nights so she can catch up.

|
|
|
|
| |
|
|
|
|
|
|
|

Poor Ella Bun. Ever since she was extubated, she is dealing with withdrawal from the narcotics. She was only on them for 4 days, but the dependence had already started. The last time she had these type of narcotics for any length of time was the NICU and they took many weeks to taper them off. Here, she was stopped immediately for extubation. In typical Ella fashion, she is not following the rules. The PICU staff is surprised by her symptoms and that she is having the withdrawal.
Last night, the Methadone was working a little bit to alleviate the symptoms of withdrawal, but she was still clearly uncomfortable. So, they started Ativan which works by slowing down the movement of chemicals in the brain. This results in a reduction in nervous tension (anxiety) and causes little sedation. They ordered a one time dose to see if it would calm her down. Ativan along with a dose of Tylenol put Ella on the right track to sleep. She actually slept last night from 11pm to 6am which was fantastic for both of us. But as soon as the action started at 6am, she has been extremely jittery and uncomfortable in her own skin. She continues to scratch herself too.
So today they are using Methadone and Ativan to control the withdrawal and keep her comfortable and Atarax to alleviate the itch. We’ve also put a hydrocortisone topical cream on her skin to help with the itch. They changed the dosage and orders so that she is getting the Methadone or Ativan once every 3 hours. We’re hoping this keeps her in a better place today. Again, they are surprised at her symptoms but are beginning to really understand that Ella goes slow and does not follow the rules.
They are going to switch her back to her home medicines today. It will be a good test to see how well her meds are being absorbed in her belly. This means discontinue the heparin drip for anti-coagulant and put her back on aspirin and Plavix via g-tube like she takes at home. She has already been on Sildenafil the past 24 hours, so they are weaning the nitric oxide throughout today and plan to discontinue overnight. She is scheduled for a repeat echo in the morning to make sure that her pulmonary hypertension is under control and that the flow in her SVC has held strong.
Respiratory wise, she had another chest xray and it looks good (not too much changed from yesterday). So they are discontinuing the IV Lasix and planning to give her hydracholorothiazide via g-tube for her diuretic, which she normally takes at home too. She has been at a flow rate of 2 liters of oxygen, so they are going to wean her to 1 liter today to see how she does (her baseline at sea level is 1/2 liter).
One thing we have noticed, once the nurse gives a med via g-tube, you can only wait about 30 minutes and then you have to vent the g-tube again otherwise Ella complains. The pressure builds up and as soon as you vent it, light green bile and lots of air comes out. This means that her guts are still not operating very much. Surgery is not surprised given the the stage of obstruction prior to surgery and that she was on so many narcotics the past few days (those slow it down a lot too). The PICU docs were pushing to try and use food today. The surgery team put their foot down and told them to wait longer. Upon examination, they can tell that her bowels are still distended quite a bit and that she needs more time.
While Ella has been at the hospital this past week, we wondered what to do with Lola. So, we found a doggie daycare nearby for her to play and get exercise during the day. They open at 6:30am and close at 7pm, so it has been nice to drop her off and not worry about her while we’re focusing on Ella’s needs. We can even watch her play during the day online via webcam.
I’m not sure if Lola just has sympathy pains for Ella and misses her, but Lola has been having symptoms for a couple of days which resulting in a vet visit this morning. She will be on antibiotics for the next 10 days. Even though she was current on all vaccinations and had her Bortadella shot for kennel cough, she must have caught a bug from one of her canine buddies. We’re hoping that Macy (the cat) does not show any symptoms and catch it from Lola. Sigh…

I’m sure it is apparent from the pictures when the meds are working to help alleviate her discomfort and when they are not. Fortunately, we have been getting little glimpses of the Bun a few times per day for about 30 minutes. Please pray for Ella’s continued comfort, for subsiding withdrawal symptoms and healing throughout today and throw a request in there for Lola too!

1 Corinthians 15:58 (NLT)
So, my dear brothers and sisters, be strong and immovable. Always work enthusiastically for the Lord, for you know that nothing you do for the Lord is ever useless.
|
|
|
|
| |
|
|
|
|
|
|
|
Who would have thought that 15 years from saying “I do” would land you @ CHOC (when you normally live in Colorado) with a beautiful miracle girl that God has allowed you to borrow for a time?
Today is our 15 year wedding anniversary. And it has been such a big day for Ella too.
Starting at shift change last night, Ella was too awake. They kept increasing the Propofol from 75 to 85, then 95, then 100. The 100 mics per kilo is the max amount for her weight. All of this over 30 minutes. Then, we tried a dose of Benadryl which has worked successfully so far. We waited twenty minutes, she was still awake. They called in the doc to double the fentanyl drip. Nothing was working to make Ella sedated enough. Even though they were pumping lots of drugs into her system, she was still fighting it. Under my breath, I’m thinking that is one of the reasons Ella has made it so far: she’s such a fighter.

Finally, they called the doc in again and he recommended a one time dose of Vecuronium (Norcuron) to deal with Ella in this acute state and get us through the night. Vecuronium is used as an adjunct to general anesthesia, to facilitate intubation and to provide muscle relaxation during surgery or mechanical ventilation. Although Vecuronium is often thought of as a muscle relaxant, it may be more accurate to classify it as a paralyzing agent. I was not real happy about giving her yet another drug, especially a paralytic agent as she is getting closer to be extubated, but I felt we were out of options.
Giving a paralytic agent reminded me of the NICU days. Not often, but more often that we wanted on some days, using a paralytic agent was the only way to manage Ella because she would fight things so much. The fact that she is continuing to build a tolerance to the sedation and waking up tells me that we need to do everything we can to get her off the vent.
While she was sedated and cooperating, she looked stable for a few hours so they drew a blood gas and then weaned the vent settings a little bit more to 14 breaths per minute around 3am. She has another blood gas at 6am and a chest xray. Her overall saturations, heart rate and blood gas will determine if she can take the next steps.
As I am every day and evening with the changes in staff, I was very specific with the nurse to wake me if there were any changes. About 4am, I awoke to beeps. They were suctioning her. I saw the nurse drawing up the Vecuronium in a vial getting ready to dispense again. I asked what was going on and was informed me that they were giving it again. With limited options in front of us, I may have opted for the same answer, but I would have liked to discuss with the doc on the downsides of giving this paralytic agent so close to her extubation. In other words, are we better to try more fentanyl or even give a bolus of versed? When was the next dose of Benadryl? Would that have been a better option? The Vecuronium held her for 4 hours, so it was probably a good call. I just got enraged over the principal: I specifically asked to be woken up with any changes or decisions regarding her care and I was not.
I went out to the charge nurse to voice my displeasure and make sure that we have a great nurse scheduled for the day shift since it is a big one for Ella. Once I calmed down enough back in the room, I went back to the room and confessed to the nurses that I was not happy. We had a nice talk about it. During our conversation they let me know that when Ella was waking again, they consulted the doc and found out that Vecuronium was ordered as needed for every hour. They admitted that they were under the impression that it was a one dose treatment as well. But they told me that they did try a bolus of fentanyl before I woke up and she did not respond. Once again, we had a clear discussion about waking me if they felt that she needed it again or they were planning to do anything different than normal maintenance and letting her current drips run. Once I was worked up, it took me a long time to be able to go back to sleep.
This morning, it became pretty apparent that it was time to extubate. Once the docs briefly took a look at her chest xray, which looked better, and watched her clinically, they started the process. They stopped the Propofol and the fentanyl. They took a blood gas which didn’t look great and she wasn’t responding to CPAP via the vent, but we think it is because she did not know what was going on with the tube in her throat and wanted it out! So, it was only about a 15 minute process and finally extubation at 8:40am! Ella did great – they did not need to bag her or put a mask on her face – which surprised them. They just took a blood gas and now she is doing better off the ventilator than on it! Praise God!
Now, the only challenge is her itchy rash on her chest area. Since she is more alert, she is itching herself and it is driving her crazy! This confirms what we thought the entire time: that she was itchy even through the sedation. We gave her Benadryl about 30 minutes ago. If that doesn’t work, they’ll need to start something else.
Otherwise, Ella is doing great on the nasal cannula with nitric oxide and 2 liters of O2. We’ll update later on this same page (remember, you will not get an email)!
I read this passage in my devotional a couple of months ago and shared it on the blog. For some reason, I felt prompted to share it again today. It must mean that someone out there reading about Ella’s story needs to be reminded of His love and His ways.
This is my doing (1 Kings 12:24).
The disappointments of life are simply hidden appointments of love.
My child, I have a message for you today. Let me whisper it in your ear so any storm clouds that may arise will shine with glory, and the rough places you may have to walk will be made smooth. It is only four words, but let them sink into your inner being, and use them as a pillow to rest your weary head. “This is my doing”.
Have you ever realized that whatever concerns you concerns me too? “For whatever touches you touches the apple of my eye” (Zech 2:8). “You are precious in my sight” (Isaiah 43:4). Therefore it is my special delight to teach you.
I want you to learn that when temptations attack you, and the enemy comes in “like a pent-up flood” (Isaiah 59:19), that “This is my doing” and that your weakness needs My strength, and your safety lies in letting Me fight for you.
Are you in difficult circumstances, surrounded by people who do not understand you, never ask your opinion, and always push you aside? “This is my doing”. I am the God of circumstances. You did not come to this place by accident – you are exactly where I meant for you to be.
Have you not asked Me to make you humble? Then see that I have placed you in the perfect school where this lesson is taught. Your circumstances and the people around you are only being used to accomplish My will.
Are you having problems with money, finding it hard to make ends meet? “This is my doing”, for I am the One who keeps your finances, and I want you to learn to depend upon Me. My supply is limitless and I “will meet all your needs” (Phil 4:19). I want to prove My promises so no one may say, “You did not trust in the LORD your God” (Deut 1:32).
Are you experiencing a time of sorrow? “This is my doing”. I am a “man of sorrows, and familiar with suffering” (Isaiah 53:3). I have allowed your earthly comforters to fail you, so that by turning to Me you may receive “eternal encouragement and good hope” (2 Thessalonians 2:16).
Have you longed to do some great work for Me but instead have been set aside on a bed of sickness and pain? “This is my doing”. You were so busy I could not get your attention, and I wanted to teach you some of My deepest truths. “They also serve who only stand and wait”. In fact, some of My greatest workers are those physically unable to serve, but who have learned to wield the powerful weapon of prayer.
Today I place a cup of holy oil in your hands. Use it freely, My child. Anoint it with every new circumstance, every word that hurts you, every interruption that makes you impatient, and every weakness you have. The pain will leave as soon as you learn to see Me in all things.

UPDATE 11:30 AM – By Josh
Well, we’re almost three hours after extubation and other than some major itchiness and a few withdrawal symptoms, Ella’s on the right path. We’re about to give her some Atarax to help with the itchiness and calm her a bit. Really though, we are all feeling relief. I think the pics below tell the story better than any words.



UPDATE 2:45 PM – By Josh
Ella is having some pretty strong withdrawal symptoms from the narcotics she’s been on for the last 4 days. She just scored an 11 on the Finnegan scale. For this reason they’re are going to put her on a low dose of Methadone. Hopefully this will ease her jitters and stop the waves of retching. We still get smiles, but we want the kiddo to be comfortable. Waiting on the dose from the pharmacy so we’ll see.
UPDATE 7:30 PM – By Tina
The initial dose of Methadone did not seem to have much effect. About an hour later, we had the doc examine her again. He went ahead and increased the dosage. The second time, she responded. We had about an hour of her still shaking a small amount, but not extreme. And she was very smiley, alert and responding like herself.
Around 7pm, she started acting agitated again. They just administered another dose of Methadone (which can be given every 6 hours) and I am waiting to see if it will calm her down again. Right now, she is resting in her bed and watching videos.
We are allowed to give the Atarax again. If she becomes agitated between now and the next dose of Methdone, we may try to see if that helps. It worked like magic the first time she took it! Plus, I do see her itching herself here and there and the red rash appears to becoming more prominent.
I’m having them order some aloe vera to put on her cheek and lips. When they extubated her this morning, they did not have orders to remove the NG tube initially. So, they retaped it to her face using a clear sticker. Her skin is so sensitive that when the nurse removed it later, it actually created little scabs on her face. Ouch!
We weighed Ella and she has lost 2.2 pounds since she was admitted last Thursday. We’re hoping that we can feed soon enough and start plumping her up again!
Thanks for all the prayer support. Ella did great today and we anticipate that she will progress forward well over the coming days. Please pray for sleep – for her and me – tonight in the PICU.

|
|
|
|
| |
|
|
|
|
|
|
|

Since we posted yesterday, lots has happened. And just so everyone knows: if you are signed up for email notifications, you will receive an email once per day when the post is first published, but then we will continue to make updates to the same post throughout the day and you will not receive more emails. You simply have to visit the website and refresh your browser to see if anything else has transpired during the remainder of the day. So for those of you who did not read the updates yesterday, you may want to!
Thanks to so many people that contacted us and networked to help out with parking the RV. As we wrote about in yesterday’s updates, we ended up having a couple of choices by the end of the day. And here is the most amazing thing: not only did the Orange County First Assembly of God provide a place to park for as long as we need, but there is 30amp electrical. Even better yet, they offered to let us refill our water this morning. When Josh explained that we would probably need to dump our tanks before we refill the water, the maintenance manager stated that we can dump our tanks at the church too! Now, how many churches do you know that have all these amenities for an RV? The Lord truly takes care of every detail.


Now, all the updates on Ella. As of yesterday when I wrote the post, Ella continued to be stable. Her fever had started to subside. The only new challenge that emerged: Ella started trying to dance a little too much! She was thrashing around so much that it was taking 3 adults to hold her down. The day nurse had given her boluses of fentanyl and versed and even increased the amount on the continuous drip. But as we headed into the evening hours, it became clear that Ella was becoming more lucid and wanted to get up and dance! It actually still seemed like she was itchy, even after we discontinued the antibiotic, so we are not sure if that was the true cause or not. The nurses can give Benadryl every 6 hours, which Ella really responds to, but then it is short lived. Finally after everything was not working, they discontinued the versed and put her on a drip of Propofol (Diprivan) @ 50 mics per kilo. Propofol is considered a general anethestic that is usually used to put kids to sleep for surgery.

The Propofol seemed to work great. She fell asleep hard and was not moving at all. Her heart rate has trended down the last couple of days from as high as 150 and is now resting in the 80s. All was great until 3am when Ella gave everyone a scare. In retrospect, they are calling it a “pulmonary hypertension spell”. Out of nowhere, she started thrashing and crashing. Her sats went down to 27 with the heart rate in the 50s. They took her off the vent and bagged her. When bagging her, they felt resistance (pressure). She did recover fairly quickly with her saturations but it took several minutes for her heart rate to climb back up to the 80s. Other than just her pulmonary hypertension, they cannot point to any other stimulus that caused the episode.

It came to light during this 3am episode with 10 people in the room as they were diagnosing, that her echo yesterday did show signs of pulmonary hypertension and mild tricuspid regurgitation. I was not aware of this fact until this time, but it started to make the picture more clear. For those of you that do not know, Ella does not show pulmonary hypertension via echos. We spent all those months in the NICU and they even told us toward the end of our visit that they were shocked, but that Ella does not have pulmonary hypertension. Then one day in the NICU toward the 5 1/2 month mark, one echo showed it. So, they gave her sildenafil and we had a new child. It was one of the biggest pieces of the puzzle to come together, making it possible for her to leave the NICU after 6 months.
When we transferred care to Denver, they ran into the same thing. She was taking sildenafil regularly, however they could never see the pulmonary hypertension on an echo. When they decided to take her off sildenafil to see what would happen, we ended up in the PICU with tricuspid regurgitation. This means that some blood leaks backward into the right atrium, increasing the volume of blood there and resulting in less blood being pumped through the heart and to the body. So, it was a bit unnerving that they are seeing both of these via the echo yesterday although it might explain this middle of the night spell. Once this happened, they decided to double the nitric oxide to help with the pulmonary hypertension. Also, they increased the Propofol to 75 mics per kilo, hoping that she would not stir again.

Ella liked her lasix and was negative for the last 24 hours with urine output by 155. So not as much as yesterday, but going in the right direction from a fluid loss perspective. Her chest xray was at 6am this morning. On rounds, they discussed that her chest xray looks improved but she still has some fluid on board. So when they came up with the plan for the day, it all revolved around extubating and take her off the vent tomorrow. We’re very excited because we’ve missed the Bun tremendously.
The docs decided that before they extubate her tomorrow, they would like to try to start giving her sildenafil again via g-tube. The surgery team gave the “ok”, but noted that unless sildenafil is absorbed via the stomach, it may not be effective given that her intestines are still shut down. The nurse gave the sildenafil and clamped off the g-tube and NG tube for about an hour to see if it would absorb.
When surgery made rounds, they took off the dressing for the incision. I was expecting a lot worse considering that the dressing was so large. Instead, it is midline but smaller than her other incision. And it appears that it is healing nicely.

Ella is still on a heparin drip for anti-coagulation. If she makes progress taking sildenafil via g-tube, they may try switching her back to aspirin and Plavix (her normal meds). For now, we’ll have to wait and see. Ella is scheduled for another echo tomorrow. It will be interesting to see if the increased nitric oxide and/or sildenafil via g-tube has decreased the pressures and reduced the amount of pulmonary hypertension.
In order to help with the acute pulmonary edema, the docs ordered Diamox (another diuretic). Ella was taking Diamox during her NICU days along with Lasix and was discharged from the NICU on Diamox and Bumex. Back then, Diamox did seem to help with getting her more dry.
They decided to give Ella a steroid today – Methylprednisolone (Medrol). It prevents the release of substances in the body that cause inflammation. They are hoping that this will help her abdominal healing.
We’re thinking tomorrow might be a big day for Ella. Please pray that her lungs are strong enough to be off the ventilator and that we can keep enough pain meds in her to keep her comfortable while awake.
Psalm 9:10 (NIV)
Those who know your name will trust in you,
for you, LORD, have never forsaken those who seek you.

UPDATE 7:15 PM – By Tina
Ella is continuing to have some strange episodes. She’s had two this afternoon and early evening since I last posted. All of a sudden, she will start “tummy breathing” which is not something you expect while she’s on the ventilator (the machine is doing most of the work). Her breaths per minute will peak at 80 breaths per minute, saturations go low, and her nostrils flare when she is breathing quickly. She’s still sedated, so it’s tough for docs to diagnose what is really happening. One time, the nurse gave Benadryl since Ella responds to that well. This last time, she could not give Benadryl because of the timeframe, so she gave her a dose of fentanyl (pain med) to help get her through the spell. Please pray that nothing major is going on that we can’t see and that she will be successful on extubation tomorrow.
One cute thing: her nurse today was pampering her and didn’t like the sterile hospital blankets. So she went back to the donation area where volunteers from Project Linus donate blankets they’ve made by hand and found one to drape across Ella. She looks so fashionista now!


|
|
|
|
| |
|
|
|
|
|
|
|


Ella was stable overnight – praise God! We had a great nurse and the doctors already started to learn Ella from yesterday, so there were no strange orders for the night. Since the nurse was so great, I did get some shut eye!
The fever is ongoing and Ella is still battling it. Tylenol seems to help keep it under control, but she still has one even as I type this update.
I did note some red rash started on her pelvis early last night. Later, it seemed to go all the way up and cover her chest. When they looked at it, they assumed that it was just a heat rash. Another symptom: itch. At intervals throughout the night and into today, Ella will move thrash around a lot and try to itch her face (maybe trying to dance?). The attentive overnight nurse put the pieces together. It appears that Ella may be having a reaction to her antibiotic, Zosin. To control the rash and itch, they give Benadryl. The rash would subside, but after the antibiotic was given, sure enough the rash starts to reappear. Fortunately, the surgery team has given the “ok” to discontinue the antibiotic today, so we’re hoping to see it dissipate.
You might notice arm guards on Ella’s arms today. The guards keep her arms extended and prevent her from itching her face and yanking any tubes. The nurse and RT are even requiring assistance with hands-on most of the time. One thing is for sure, she is a fighter!

There are new docs on this morning. I wish we had the one from yesterday – she was amazing. I think she had lots of experience with pulmonary hypertension patients and had a great respect for moving slow. As all of you know, Ella responds best that way. The docs this morning came in talking about taking her off the vent and extubating her. I asked if they had taken a look at the chest xray from this morning. They had not seen it yet, but stated that most kids come off the vent in 24-48 hours. I took a deep breath and realized it was going to be one of those days.
I fought for leaving her on the vent. I know that Lasix has done really well and that she is negative 675 for the last 24 hours, but she is still 2 liters positive since she was admitted. In real language, this means that she has peed a lot in the last 24 hours (more than what she has taken in by 675ccs), but she still has a lot of fluid on board. Sure enough after looking at the new chest xray, the doc came back and agreed that there is no doubt she needs to stay on the vent for another day or so (ya think?).
All their intentions are good, but it is frustrating when they want to use standard care protocol that they follow with normal, healthy kids. They expect that because Ella’s numbers look good in that moment that she should follow all those same guidelines. As her parents, we’ve learned to go slow and give her more time. You should be 110% sure that she is strong enough and ready for the next step. In this case, she has had major abdominal surgery and is contending with enough much less breathing when she still has fluid on her lungs. Sometimes docs just want to move too quickly. I felt like the PICU doc yesterday understood really well, but not as much the ones today.
I think they are planning on starting heparin this afternoon since it will have been 48 hours since surgery. They will use this as her anti-coagulant for her SVC, until she is ready to take her regular medicines.
Surgery came by and was happy with how she looked. There is still a good amount of bile coming through the NG tube (the tube in her nose) and her G-tube (the tube in her belly). Once there is little to no leakage and/or the liquid is clear, we should start to see her bowels working again. So, likely another 3-5 days. The surgical nurse practitioner explained that once the intestine has gone through surgery, it closes off temporarily and slowly opens back up for operation. We’ll be looking for passing gas or bowel movements in the days to come.
Ella had another echo this morning. The goal is to check to make sure her cardiac function is good. If all looks satisfactory, they will discontinue the Mirilone (heart medicine) and just use Nitric Oxide to keep her pulmonary hypertension in check.
Overall, Ella looks pretty good. We’re just trying to let her rest, get more fluid off of her (big surprise) and keep her comfortable.
Thanks for all the support and prayers – it means so much.
One last item: if you remember, we came to CA on a road trip in our RV. The hospital does not have any place to park the RV. After Josh dropped me off at the ER with Ella, he drove to the closest location where he could maneuver, which was the Main Street Mall (just across from Macy’s). He got permission from security to park there a few nights, but they are not keen on us continuing to stay. We’ve tried the church connected to St. Joseph’s, the Ronald McDonald House, the closest Walmart, various RV parks close by (too pricey plus not real nice/secure). For one reason or another, none have worked out. But now we figured that we would reach out to those locally, as you may have an answer for us! Does anyone know of a church or business near CHOC that would allow us to just park the RV? We take up 2 parking spaces. We have our dog and cat with us, so we need someplace secure and where we can walk Lola. Fortunately, Josh’s aunt did loan us her car, so the RV does not have to be right next to the hospital although that would be ideal.
UPDATE 3:15 PM – By Tina
Josh went and pleaded again with the hospital security crew for a place to park the RV at the hospital, the sisters at St. Joseph’s, and visited other places nearby to research while I’ve stayed at the ICU with Ella. Those attempts were not successful. Another place I thought to look: the Crystal Cathedral. It is less than a 10 minute drive and they have lots of room. Josh just sent a text to my phone letting me know that we can stay there for up to 3 weeks!!!
UPDATE 5:30 PM – By Tina
And now, Josh just called because another brother in Christ has been fervent on the phone and has found another church that is willing to let us park the RV for as long as we need (Orange County First Assembly of God, www.ocfirstag.org). Yes, God is continuing to provide in the midst of the storm. Thanks to everyone that was providing ideas and trying to help us. We will update later with the spot where we’ve landed.
Psalm 46:5 (NASB)
God is in the midst of her, she will not be moved; God will help her when morning dawns.

|
|
|
|
| |
|
|
|
|
|
|
|

Ella had a fever last night, but it finally broke early this morning. As her mom, I stayed up pretty much all night to oversee the management of her care. Right off the top, I will say that we have been impressed with the staff at CHOC. They are doing a good job of taking their expertise and listening to us as her parents that know Ella, to come up with a plan.
Last night was the first night post surgery with the night crew and people that don’t have Ella experience. We did our best to warn them about her sensitivity to fluids and that they may want to consider giving diuretic in the OR or shortly thereafter to maintain her fluid status. The surgical team is worried and does not want to give diuretic because they need to make sure that her intravascular system is not too dry. Yet, we know that if you go too long and let her get too wet, you will have lots of other issues to deal with besides her surgery recovery.
It has only been about 20 hours since surgery and they have started to learn to listen to her parents and the Denver docs input. Overnight, the docs were a bit too aggressive in trying to wean her and give her fluids. I was suspect, but wanted to let them get a feel for her and her responses. I did put my foot down when the overnight doc wanted to cease her nitric oxide. Since we were admitted, they stopped giving her sildenafil which she normally takes to control her pulmonary hypertension (they didn’t want to put anything in her guts and sildenafil is not available via IV). So, they opted to manage her pulmonary hypertension with the nitric oxide. Last night, the doc wanted to cease the nitric oxide because “she looked good”. I was adamant and won that battle.
Her urine output has been low. This is not surprising because she usually requires diuretic every day to keep her dry. At this point, they had not given her any diuretic. Like they would treat a normal case, they suspected that she was not peeing because she was too dry. I highly doubted that she was too dry, but wanted to give them the freedom to manage her. So, they gave her two boluses of fluid to try and encourage urine output. As I expected, no true urine output. After advocating, they gave a half dose of lasix via IV (which Ella usually likes), and she gave out 300ccs of urine! This was before they took another chest xray. Then at 5:30am, they took another chest xray. Josh and I both took a look along with the docs – I think it worried them a bit. She is very wet.
This was their first introduction to Ella and her fluid sensitivities. I called her pulmonologist in Denver, who is amazing and always makes himself available, and he gave his cell phone so that the docs at CHOC could consult with him on her fluid sensitivity and the best plan for management if needed. But before I gave them the number, the new doc in charge for the day in the PICU was already putting the pieces together which was impressive. She increased her nitric oxide, increased the ventilator settings (which had been weaned with the overnight crew), increased orders for sedation, and ordered a full dose of diuretic once every 6 hours. She mentioned a lasix IV drip. We explained that Ella tends to respond to bolus lasix better (hitting her kidneys all at once in short boluses versus a drip gives more urine output). She took in our input and changed the order which is so appreciated.
The head of cardilogy came by for a visit. He has been incredibly valuable in managing the heart and lung issues pre-surgery, surgery and post-surgery. He is the one that decided to give her nitric oxide for her pulmonary hypertension, after consulting Ella’s Denver docs. This morning, he also added Milrinone, which is a medicine that they give a lot of times to kids with a weakened heart. It will simply supplement the nitric oxide and help her heart and lungs function together. Ella has not been on this before (to our knowledge), so it will be interesting to see her response.
They consulted hematology because they want to make sure that her blood clots enough for her new abdominal scar to heal but not so much that it impacts her SVC from clotting off. So, they noted from her earlier labs that her AT3 (Antithrombin 3) count was low. This is a protein in everyone’s blood that naturally helps with clotting. Hers was 116 before surgery. This morning, it was in the 60s. They want to see it maintain 100+ throughout today, so they gave her a dose and will monitor with labs. Tomorrow, the surgical team has given the “ok” to start Ella back on a heparin drip to make sure that the SVC is not impacted.
The surgeon did come by and confirm that yesterday went very well, but her intestines were so tense and dilated, it would not have been too much time before they burst. Initially, we were just told that they would not burst but that the tissue would just die. She reiterated that her intestines would have burst which would have been deadly for Ella. Wow, how the Lord takes care of and protects this little girl…it is truly amazing.
Today’s goal is a day of rest for Ella and reducing the amount of fluid in her lungs while her abdominal scar heals. Thanks for all the love and support.
p.s. As a side note (for those of you that don’t know), when we post an update for the first time each day, you will receive an email. But as we update throughout each day, you will not receive another email. So, you’ll need to just check back every so often to see if there has been another update.
Proverbs 3:5-6 (NIV)
Trust in the LORD with all your heart
and lean not on your own understanding;
in all your ways acknowledge him,
and he will make your paths straight.
|
|
|
|
| |
|
|
|
|
|
|
|
Ella and I both caught rest last night, as the situation would permit. Being in intensive care means that they have to conduct vitals once every 2 hours. Each time they came in and started touching her, she would wake up and cry. Then, she kept crying because she was in pain. Now, the window between doses of Morphine has narrowed to once every two hours. If we don’t give her the morphine, she can’t sleep due to discomfort.
I wish that she was not outputting as much bile, but in fact she did output about 500ccs of dark green bile from her g-tube. The last time she passed gas or had a bowel movement was Wednesday morning. She had repeat abdominal films this morning – they are unchanged from yesterday. This is better than them looking worse although clinically, she is doing worse. She is in more discomfort and requiring more pain meds. Her belly is more distended. Last night at shift change they measured her belly and it was 1.5cm larger this morning. She is going in the wrong direction.
Upon exam this morning, the surgeon did a rectal exam to see if there was any presence of stool. His glove was clean when he pulled his finger from her rectum – not a great sign. If there was some presence of stool, they might try giving laxatives to help push it along. But if the obstruction is in her small intestines and is a full obstruction, giving laxatives is not going to help.
It is such a hard call for them. I think if she was a healthy toddler without other complications, the surgery would have already taken place. The first films on Thursday showed 6-7cm of dilation in her small intestine, which even in an adult, is huge and warrants immediate surgery. But because of all her other health complications and the fact that she was taking anti-coagulants as part of her daily medicines (aspirin and Plavix to help her heart stents remain open) caused great concern for the surgical team. With anti-cagulants in her system, it is a huge risk for bleeding in surgery. So, they opted to place her in intensive care and watch closely to see if rest for the intestines would lead to an improved status. The films on Friday looked better than Thursday, but still not good. Today, they look about the same as Friday. I’ve been told that they are coming by in about an hour to discuss which plan of action: wait longer or try surgery.
Thanks for all the prayers for sweet Ella. And please pray for me and Josh – it has been emotional to realize that she may need another major surgery – she’s been through so much already. It’s been even more difficult since we are at a hospital that is not familiar with Ella. We’ve been through this before when we first came back to Denver and Ella needed surgery. At that time, only Shands and Dr. Kays knew Ella.
We know that ultimately He is control. The Lord decided that this was the place for Ella to be when this obstruction happened. The truth: He orchestrates and authors every detail, only wanting the best but allowing whatever is necessary for His glory. Right now, we look to Him for our comfort and knowledge that whatever may happen, He is in charge of all the details.
This doesn’t make the emotional part any easier, so please pray for us as parents that He will equip us to make decisions for Ella today. And please pray for the doctors involved in this decision-making process – that they will have unsurpassed knowledge and discernment for Ella’s needs.

UPDATE 12:00 PM – By Josh
It’s time for surgery. It is more serious than expected. They’ll be doing a midline incision…didn’t expect that. There’s even a possibility of reherniation of her diaphragm. They think they might see some loops of intestines in her chest. Please pray for our sweet girl to stay strong through this process. She will be intubated for awhile as well. They have indicated this is a very big surgery, very high risk, and multiple issues to contend with.
Heavenly Father, we trust in you, we rest in you. Please watch over our precious child. She is your sweet girl. Her life for your Glory. Thank you Jesus. Amen.
UPDATE 7:30 PM – By Tina
WARNING: THERE ARE GRAPHIC IMAGES BELOW.


Thanks for all the prayers. Ella came through surgery like a champ. There is no question that she needed the surgery. It was confirmed that there was a large obstruction in her small intestine. The small intestine was very swollen and distended causing the large back up of bile and all of her discomfort. We are so blessed that they did not have to cut or resection the intestine. They pulled out her entire intestine to check all of it. None of it had died, so they did not need to cut any away. Instead, they just made a small incision and flushed out her bowels. The obstruction was in the small intestine, near her spleen. The surgeon noted that this was likely a problem that had been occurring for quite some time due to the scarring on the intestine. We have had small incidents like this before and that was a red flag that an obstruction was likely in our future. In previous days, it would resolve on its own without surgical intervention. Today confirmed that the surgery was absolutely necessary.


From the xrays, they thought Ella might have re-herniated her diaphragm. Thankfully, the gortex patch is still intact with scar tissue covering it (Thanks to Dr. Kays!). However, there was a portion of Ella’s intestine that was stuck to the diaphragm area which confirmed what they noted on film. Although this was not the area of obstruction, it may have become an area of concern, so they addressed that as well.
Ella is not out of the woods. The next 48 hours are absolutely critical. They expect her to get puffy and swollen and not look too good. She is intubated and on a ventilator. This was major abdominal surgery where they completely removed her entire intestine. Her body is going to be angry for a couple of days before it settles down and starts recovering. We just need to pray that she can maintain her fluid status (the docs here have not experienced Ella and fluids), and that she remains comfortable.
Thanks again for all the support and prayers. Our sweet little Bun is doing well and both of her grandmas are at the hospital this evening to provide support. We’ll update again tomorrow.

UPDATE 9:30 PM – By Tina
I thought that I would not update until tomorrow, but I did want to share that Ella has a temperature of 102.7 degrees. It might be a rough night. Please continue to pray for her!

|
|
|
|
|
|