| |
|
|
|
|
|
|
|
It was another great day with the Bun.
We took a field trip down to the Super Target near the house. We are not really supposed to go inside with her, but it was a necessity. Since we were at the hospital last week and Josh is out of town, the refrigerator and pantry were empty. I could have likely eaten cereal for 2 days, but we were out of nursery water for Ella’s formula. So we took the plunge and walked to get some groceries. I opted to use the Baby Bjorn and give Ella a view of her surroundings. This way, the oxygen tank and groceries could be place d in the stroller on the way back.
It was a beautiful day outside, nice and sunny. Ella sported her navy dress with a cap and sunglasses. She looked adorable. It was great exercise for her to hold her head upright while we walked. Plus, it was unseasonably hot in Colorado for the past few weeks. So we have not taken a walk in a long time. Today, it was a normal temperature. The high was 88 and it has cooled down to 69 degrees this evening. It was nice to get outside with her again. I think she really likes it.
We heard that a new PT and OT have been assigned to us from Developmental Pathways. It will be interesting to see how things go over the coming weeks with the new therapists. And although it will not be quite as consistent, we are still going to try and pursue a different PT and OT through a home health care agency too. Between therapy from both angles, we should be able to give Ella what she needs.
Tomorrow, we get to go back to the Children’s Hospital for blood labs. They want to check all her electrolytes and other levels. It will be interesting to see where her BUN falls. I think it might be a tad lower than the last draw which was 23. But we’ll see.
Once we’re done with labs, we are going to see Dr. Perry. We haven’t seen him since a week ago. He went out of town last week, so we did keep in touch with colleagues from his practice. But it will be good to see him again and come up with our plan for Ella over the coming weeks.
When I put Ella to bed tonight, she was still on 1 liter and saturating 100%. I may try weaning her oxygen once she is really asleep. This way, I can see if the extra oxygen is truly making a difference. It seems like she might be ready to go down a little bit since she has been at 1 liter for 3 days now.
The picture below is so cute. This was earlier in the evening when she decided to take a snooze. I just love how relaxed she is and that she likes to cross her legs, even when she is catching up on beauty sleep.
We’re missing Josh and can’t wait for him to come home.

|
|
|
|
| |
|
|
|
|
|
|
|
Today was a relaxing day at home with Ella.
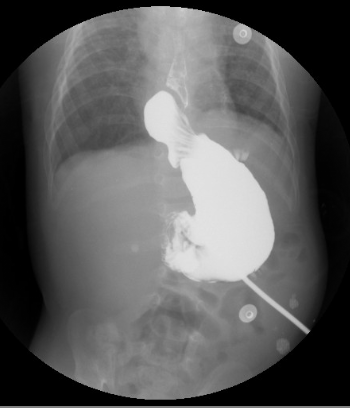
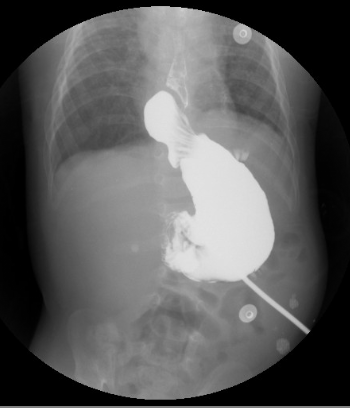
She did really well last night sleeping in her own bed. Our pulse oximeter showed similar saturation and heart rate that mirrored the hospital. This is one of the best ways for us to keep a close watch on Ella’s fluid levels. Last night, she was saturating 100% and her heart rate was between 85-105 when she was in deep sleep. She is still on 1 liter of oxygen. If she does well tomorrow, I think we will look to wean tomorrow night again, once she is asleep.
As I type this, it is raining really hard in the metro Denver area. There is lots of thunder and lightening. I hope it does not wake up the Bun. It is very loud; it has made me cringe a few times. When I ran into her room to shut the windows, her saturation was 100% and her heart rate was 92. This is really good and so different than the week prior.
In the midst of Grandma West visiting and then going to the hospital, I neglected to mention about Ella’s therapy situation. We have been going through the Early Childhood Intervention program for OT and PT. Well, the OT that was assigned came for 2 appointments. By the last appointment, it was evident that it was not a match. I’m sure that she was very qualified, but she rubbed me the wrong way. Personality-wise, she had an abrasive edge to her. So, I asked our case manager if we could find someone else in their network to work with Ella.
Then, last Saturday before we went to the hospital, Ella’s PT called and explained that she had a personal situation arise and needed to cut back her work schedule. So, she dropped us off her schedule. Along with needing to thin out her schedule, I also think that Ella was a lot of work and a great challenge for this therapist. We really liked her, so we’re bummed that we have to find another one.
We started this process when we came back on June 1st. Two months have passed and Ella has not really gotten any great therapy sessions. We have not made any progress forward for Ella for OT or PT. I just feel like we made such great progress in the 4 months post-hospital in Gainesville. Now we are having a tough time getting into a groove for therapy in Denver.
I am planning on getting services through the Early Intervention Program, but have decided to pursue therapy through our health insurance benefits again too for the majority of the sessions. I just feel like the therapists are way better and more experienced. It is strange to me that we ended up with 2 great therapists in Gainesville and now that we are back home in Denver (in a major metro area), we are having trouble making this happen.
Also, I mentioned before that we were trying to get private duty nursing hours. A few weeks back, our health insurance company authorized 20 hours per week for the first 30 days and then re-evaluate. We have been through 7 health care agencies and no one can staff. There is such a shortage in certified nurses through the health care agencies, especially those that work with pediatric patients. So, we have not been able to take advantage of this benefit. Hoping and praying that it will work out, if it is meant to be. It would be nice to have a break here and there.
I made contact with some NICU nurses today and found out that Dr. Kays is on vacation. He is not expected back until August 18th. So, we will need to be patient and wait for his opinion.
Listening to Charles Stanley this afternoon, I am reminded of four truths about God. First, that God is in absolute control. He controls all the circumstances in our life. Second, He will always meet our every need (things that fit into His will and purpose for our lives). Third, God is always with us (nothing will ever be able to separate us from the love of God). Lastly, that He loves us eternally. All of these truths mean that even when the circumstances of life are not the best, we can have confidence.
Please continue to pray for Ella and her health – that she will remain strong. Also, that the best therapists will be placed in our path. And finally, please pray for our upcoming decisions regarding her surgery.
Psalm 68:19
Praise be to the LORD, to God our Savior, who daily bears our burdens.

|
|
|
|
| |
|
|
|
|
|
|
|
Man, this hospital is nice…and the views aren’t bad. A nice touch when you are pondering things and going through something heavy.
We left the hospital about 2pm today. Yippee! It is good to be writing this post from home this evening.
Ella did incredibly well last night. She slept solid the entire night. I thought the steroids would keep her up for a 4th night in a row, but I was pleasantly surprised. She slept from 9pm – 9am; I am sure she was exhausted from her lack of sleep these days too. I slept from 11pm – 6am, but those 7 hours felt like a dream!
Wow, I am not sure what happened. But Ella’s heart rate last night and this morning while she was relaxed and asleep were the lowest numbers I had ever seen. The only time the numbers have been even remotely close is mid-January in the NICU after they introduced sildenafil for the first time. This morning, I had to take a video so I can prove it to Josh. Her heart rate was fluctuating between 85-105. I have never seen them dance in the 80s before, ever. I knew that meant that she was very relaxed and had to be feeling better.
About 9pm last night, I weaned her oxygen down to 1 liter. She usually saturates incredible while she is sleeping – – it is always the awake time that is more dicey. But this morning, she was saturating well on 1 liter while awake too. Some might have argued to keep weaning, but I think the key with Ella is slow. So, we will likely stay on a liter for another 2-3 days. I want her to be rested and ready. Because we have not established a true baseline for oxygen requirement in the altitude and we want to be more on top of it, we may have to use a pulse oximeter during the daytime too so we can monitor and adjust accordingly.
We ordered a DVD from Shands to upload all of Ella’s medical records into the system at the Children’s Hospital in Denver. Unfortunately, they were having a tough time loading the images into their system. Josh tried viewing the images on my computer and it worked. Since I had the images handy, I thought I would show everyone some images that relate to this recent hospital stay.
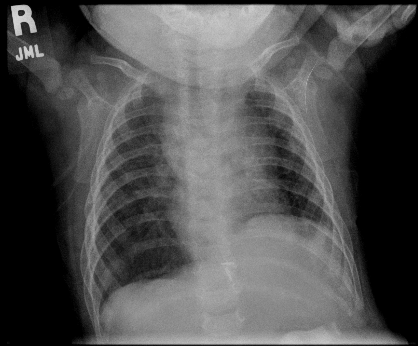
This is a picture of Ella’s lungs back in mid-May right before we left Gainesville. She was more “dry” during the time of this xray.
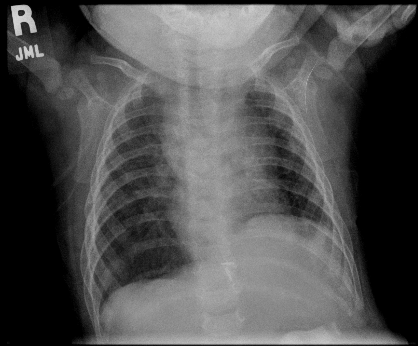
Below is Ella’s chest xray from Monday, August 5th when she was admitted to the Children’s Hospital. You can see that the film is hazy. This is what Ella’s lungs look like when she retains fluid and is more “wet”.
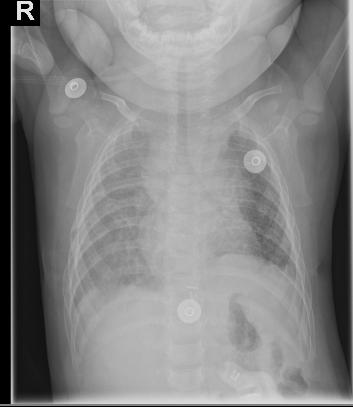
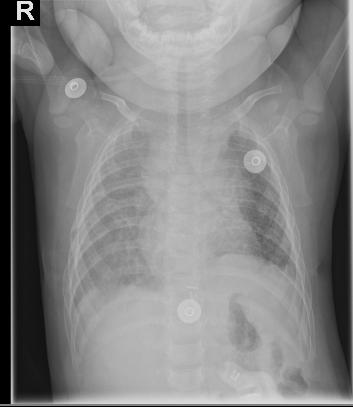
Also, below is a picture of Ella’s hiatal hernia. So you can see her stomach filled with the barum fluid that radiology uses for contrast. Above and to the left, the round ball shape is the nissen fundoplication or nissen wrap (where Dr. Kays tied the lower part of her esophagus to the upper part of her stomach), to prevent the reflux back into her esophagus and prevent aspiration. While the wrap still looks intact, it has herniated above into her chest through the hiatus (the natural opening in the diaphragm where the esophagus lies). So now it is above her diaphragm area resting in her chest against the side of the esophagus. This is why they think that she might be gagging and retching more than normal.
Speaking of retching, she has not retched a single time today! Again, she is more dried out and I don’t hear her wrestling with any secretions, which is a nice change. I would love it if we could keep her dry enough to not have to battle constant secretions.
Ella is sure feeling more like herself today. It’s so nice to see those smiles!
Another day has gone by without hearing from Dr. Kays. All I can think is that he is super busy. I’m hoping to hear his thoughts soon.
Our neighbor showed our house for rent this evening (and continues to mow the lawn for us – they’re saints!). We’re still praying for the right tenant to occupy our home. We know that He has a plan…we’re trying to be patient and trust.
Finally, thanks for all the prayers. The support means so much during times like this past week.
James 5:11
As you know, we consider blessed those who have persevered. You have heard of Job’s perseverance and have seen what the Lord finally brought about. The Lord is full of compassion and mercy.

|
|
|
|
| |
|
|
|
|
|
|
|

…I love ya tomorrow, your always a day away.
Ella was up again all last night. She finally went to bed at 5am and we both slept until about 7:30am. I’m hoping that tonight is better, but I don’t think it will be. Those steroids do a number on her. They will be over in a couple of days – thank God.
Today was a good day for Ella. She made steps in the right direction. Her oxygen was at 1.5 liters most of the day and she remained stable. I decided to take over the weaning of the oxygen. I felt like they were weaning too fast and I could start to see the signs early when they were being too aggressive. Right now, Ella is taking a nap (I just fed her and administered the steroids so they have not kicked in yet!). Since she is sleeping, she is totally relaxed and requiring less oxygen. She is at 1 liter and saturating 100%, which is good. I expect that I will have to increase the oxygen while she is awake and fussy tonight, but I can tell that she is getting stronger. It will just take her awhile to get lower on her oxygen requirement. The good news is that we don’t have to stay in the hospital to make that happen.
She was poked again today for her labs. All her levels were reasonable, including her BUN which was 23. So, her BUN went from 14 on Monday to 28 on Wednesday (after being given megadoses of IV lasix and Bumex), and was 23 today on Friday after adjusting her Bumex dose for her weight.
The other observation: since she really dried out over the past day or so, she has not had a lot of secretions. We were getting to the point where she was having such thick secretions frequently and she did not know how to manage them. Therefore, she would cough, gag, retch. She was doing this 10-40 times per day. The interesting part: she has not been retching hardly at all since she has dried out.
Ella has been letting me know the past 2 days that she is dying of thirst. Finally late today, we got the okay from pulmonology to give her 4-8 ounces of water per day, as she desires. It’s been hard because I have been unable to give her anything via mouth. Yet, she is asking for it by opening up her mouth wide and complaining. Along with it being dry in Denver, the steroids can cause dry mouth. As soon as I could today, I gave her some water. She was a happy girl; she wanted it so bad. She took 4 ounces without a problem. Another highlight: she never retched. She has been retching with oral intake of fluid for the past few weeks, so it was very promising to see. Could this mean that retching is tied to secretions which is better/worse depending on how wet/dry she is at any given moment? Hmmm…
Grandpa visited her today. He has been tired too, so I caught him catching a few zzzs while I was talking to the in-house physical therapists.

As long as Ella can remain stable tonight, even though she is at a way higher oxygen requirement, they will discharge us tomorrow! This means that we can go home, let Ella get better and slowly wean the oxygen as we see necessary. Josh went out of town this evening and will be back late Tuesday evening. He was a bit hesitant to leave his girls, but I convinced him that we would be okay. Plus, we have Grandpa and lots of friends we can call on if we need help.
With a discharge from the hospital, it will mean that we have to come back to the hospital early next week for labs again. They will want to check all her electrolytes as well as her BUN to make sure that she is staying dry on her increased dosage of diuretics.
After speaking with the surgeon tonight, it is looking like we will need surgery to repair Ella’s nissen. If you remember, she has a nissen fundoplication (she underwent a surgery that took the upper part of her stomach and wrapped it to the lower part of her esophagus. This is a permanent surgery that was completed last Nov 2007 and was done to prevent her moderate to severe reflux as well as help prevent aspiration).
The upper GI results from the other day show that she has a hiatal hernia.
Mayo Clinic describes it this way:
“The exact cause of hiatal hernias isn’t known. Your chest cavity and abdomen are separated by your diaphragm — a large dome-shaped muscle that’s responsible for a major part of normal breathing. Your esophagus passes into your stomach through an opening in the diaphragm called the hiatus. Hiatal hernias occur when the muscle tissue surrounding this opening becomes weak, and the upper part of your stomach bulges up through the diaphragm into your chest cavity.”
Her nissen wrap has migrated above her diaphragm into her chest cavity and is currently pushing into the side of her esophagus, thus causing difficulty swallowing, gagging, retching and a potential over time to begin causing reflux.
This is not a surgery that is critical and needs to be done ASAP. We should wait until Ella is stable with her lungs and fluid issues. But there are consequences for waiting too long: the hiatus hernia can get bigger and portions of the stomach can migrate into the chest cavity too. Also, it is likely that Ella will continue to have the cough, gag, retch and swallow difficulties. They don’t really want us to pursue oral feeding therapy until it is repaired. With this in mind, we should consider having surgery in the next few weeks.
We are still waiting to get a second opinion from Dr. Kays. Based on what the surgeons here are telling me, she does not have a subtle hiatal hernia. It is easily noted on the radiology images and therefore, it is likely that Dr. Kays will agree with their recommendation(s).
Again, please pray that Ella continues to go the right direction and that she can strengthen. We would really like to go home tomorrow, if possible. Also, that Josh and I will have wisdom and discernment to make the right decision for Ella concerning her surgery, down to every detail.
Lamentations 3:22-23
Because of the LORD’s great love we are not consumed, for His promises never fail. They are new every morning; great is Your faithfulness.
|
|
|
|
| |
|
|
|
Posted ( jooosh) in All Posts on August-7-2008 |
|
|

Yeah…that’s what I said…surgery. You can see by the look on Ella’s face she’s not too excited either.
I’ll get to that in a minute, but first let me bring ya’ll up to speed. Although I had a work project and couldn’t get to the hospital ’till midnight, I gave Tina a break so she could go home to sleep while I spent the night with Ella.
Once again the prednisolone kept Ella up pretty much all night. She was restless and woke up about every 15 minutes. She finally went to sleep around 5:00am but only for about 45 minutes or so.
Her oxygen was also weaned down to 1 liter last night, and she seamed to be tolerating it ok. She took a long 3 hour nap in the late morning and during that time her heart rate and saturations looked great. Her heart rate hovered around 105 bpm and even dipped as low as 89!
Later in the afternoon Ella started having some problems breathing. Her breaths became more labored and she started getting upset. I let the nurse know what was going on and we began to increase her O2, both in her cannulas and with blow by. Ella had a real hard time recovering but she finally did. We think we figured the cause of this one though. We believe that Ella’s O2 is being weaned too fast.
When she was on a liter of O2, her saturations hovered in the mid 90’s but would dip into the low 90’s as well. When this would happen her body would try and compensate by working harder to maintain the higher saturation. By the afternoon, she was just worn out which caused her to spiral down. We know Ella likes to take her time with things, so moving forward we will be weaning her slooowly so we don’t encounter this again.
Also, Ella had her swallow study done. It wasn’t real bad, but it wasn’t perfect either. The good news is that she is not aspirating immediately when she swallows, but her timing is off enough to where the food is being stopped by her vocal cords and muscles in her throat instead of the epiglottis. We’ll find out in the coming days the recommended approach for giving her food and drink orally.

Ella had an EKG done this evening just as a precautionary measure because her heart rate monitor kept throwing these weird alerts. The doc didn’t think she was actually experiencing them, but just to be on the safe side, she wanted a test done.
The big news of the day though relates to the upper GI study they did the other day. If you remember, the technician told Tina that everything looked ok. But after the radiologist studied the images in detail, it looks as though Ella’s nissen has pushed past her diaphragm and is up in her chest area. This is the most likely cause for her increased retching when she drinks or starts to cough because it’s pressing against her esophagus.
Repairing this will require surgery…something we’re really not excited about to say the least. We still have not talked about all the details with the surgery team, and we’re also waiting to get a consult from Dr. Kays before we do anything. The earliest the surgery would even take place would be the middle of next week, but we’ll just have to see. I just know that with all of Ella’s history, no surgery is going to be very straightforward.
Even with all this, Ella is taking it in stride. She’s seems to be feeling better tonight, even acting more like herself.
Please pray for our girl in the coming days and for wisdom so that path is made clear for the doctors and in our decisions.
Praise God for this sweet little Bun.
|
|
|
|
| |
|
|
|
|
|
|
|
UPDATE – 1:20AM (MST): Ella is not sleeping well. She is going in and out of sleep with a bit of fogginess. She seems disoriented. This is new. I wonder if it is the steroid that she received at 6pm; she’s never had that drug before tonight (Prednisolone). The nurse stated that they give this med to asthma patients frequently and it can have a restless effect. I know that she is overtired, but something seems different. She was crying like she was in pain and would not take her binky. I hope she isn’t working too hard.
Also, they decided to give her IV lasix at 12:15am; she’s had one diaper weighing in at 115. Anything over 100 is a good output for her.
On a positive note, her heart rate is around 110-115 and she is saturating 100 when she is still and asleep. I have not seen her heartrate that low in several weeks. I just wish I was seeing those numbers while she was on her baseline amount of oxygen, but she is still at 2.5 liters. Please say a prayer that she will go to sleep and rest soundly! She is so tired…and Mommy is too!
UPDATE – 2:40AM (MST):Yep, we’re still up. Ella is continuing this strange behavior, on and off about once every 15-25 minutes. They tried giving Tylenol earlier at 1:20am, but it didn’t seem to do much. The doctor gave her another full examination and thinks that she looks fine. She simply attributes it to a combination of possibly the steroids, but mostly that she is sick, doesn’t feel well and maybe has an overall achy feeling. Please pray that Ella can sleep away her discomfort and that there is not something else going on!

UPDATE – 8:45AM (MST):Ella and I did not sleep well last night. I’m convinced that it is the steroids that kept her up and had her feeling jittery and uncomfortable (look at that hairdo!).
We were woken up at 6am because the night shift team wanted a blood gas and so they wanted to poke her again. Literally, she has been poked 10+ times in the last 48 hours. I guess her potassium was a bit low yesterday and then they gave her lasix, so they want to check the levels again. Since they have used all good veins, they ended up trying in her hand and resorting to a heel prick.
I’m pushing for a plan and strategy today from the day shift team. I don’t feel like we have one central point of contact. And at this time, I’m not clear on what their goals are for her over the coming days. Do they want a clear chest xray? Do they simply want her saturating well with a good heart rate at her baseline of oxygen requirement? Are they going to give her more diuretics? Are they going to want more blood gases? What are our goals for her? All of the above? As you can see, I’ve got lots of questions. I’m hoping the day shift team can help answer them today.
Although we had a rough night, she is looking a lot better this morning. She is down to 1.5 liters of oxygen. She doesn’t seem to be working as hard. Right now, she is watching a video in her crib – her heart rate is 128 and she is saturating at 97-98, with some feet kicking going on. Yesterday, her heart rate when she was awake was around 175 for most of the day.
She still sounds sick – congestion and coughing. But the fact that she is not working as hard makes me feel better.
I feel like the fluid issue is subtly being confirmed. They gave her an extra dose of Bumex yesterday as well as IV lasix. Her urine output on Monday was ~300ml. Her urine output yesterday with the increased diuretics was 535ml. So, she definitely is getting rid of some fluid (normal range for her would be 168 – 336; 1-2mls per kilo, per hour).
The fluid theory is also being confirmed when you look at her weight. She weighed in with the ER at 16 lbs 4 oz (7.47 kilos) and this morning she weighed 15 lbs 6 oz (7.1 kilos). That is a big weight shift between Monday morning and Wednesday morning.
Looking back, she weighed 15 lbs 12 oz at Dr. Perry’s office a week ago on Monday (one week prior to being admitted), so she may have been retaining fluid at that point too.
The night shift resident really rubbed me the wrong way last night. She came off as abrasive and you don’t get the feeling that she respects a parent’s input. For example, Ella was really fussy and it took a long time to get her to sleep. The resident came in and wanted to “listen to her”. That process wakes Ella up. Since she was saturating beautifully and there was nothing clinically to indicate a crises, we asked if she could hold off on listening. We got an attitude and she basically disagreed and said that she was going to listen to her anyway. Sure enough, it woke up Ella.
Fortunately, I’ve really liked the day shift team, so I’m going to focus my efforts in getting a plan in place today.
Please continue to pray that Ella will feel better. Also, that her and I can catch some naps throughout the day so we are not feeling so sleep deprived.
UPDATE – 10:30PM (MST): Thank you for all the prayers. Ella and I did catch a few short naps today and they definitely helped! Also, I think that Ella is so tired that she has actually been sleeping really well this past hour or so. I hope that is indicative of how she will rest for the remainder of the night.
Today was mostly a resting day for the Bun. They have left her on 1.5 liters of oxygen, but she has been stable and saturating beautifully all day long. I am sure that they will wean her at some point this evening or first thing in the morning.
She has gotten dry – this is why she is starting to feel better. The increased dosage of bumex and the shot of IV lasix has helped reduce her fluid. Her BUN on Monday was 14, it was 19 yesterday and this morning, it shot to 28 which is really dry. I think the increased diuretics along with the steroids have done the trick. In the past, we have only used diuretics and it has taken several days for her to dry out. The steroids shortened the life of that real quick, which is great because it means that Ella must be feeling better. She certainly isn’t laboring as hard to breathe.
Her swallow study is scheduled tomorrow. We should also hear back from pulmonology and gastroenterology regarding the next steps that we want to take with her care. Today was a lot of me pushing buttons and becoming a squeaky wheel to get them to understand that we need a plan. I think the pieces of the puzzle will start coming together tomorrow and the picture will be more clear about next steps.
Josh is working late tonight, but will be reliving me at some point. In the meantime, I’m going to shut my eyes and catch some zzzs right now. Later, I will dash home and sleep in our bed to get caught up on sleep and Josh will stay overnight with Ella.
Please pray that Ella sleeps well tonight…that will make for a much happier Daddy. Also, that we can consult with the various departments tomorrow and get the wisdom from all the doctors so that we can come up with a plan for Ella….a plan that we will feel comfortable with implementing.
Thanks again for all the support and prayers.

|
|
|
|
| |
|
|
|
|
|
|
|
Sorry for the delay in updating today. It was a packed day for me and the Bun.
Ella slept well last night and seemed to be stable, so the nurse reduced her oxygen to 750ccs. Once she woke up, I expressed to the nurse that it seemed like she needed more O2 while she was awake. So, the nurse put it back to 1 liter.
We went down to radiology at 10:15am. Too bad I did not have a camera of Ella riding in the Red Wagon down to her procedure. It was pretty cute. She sucked her binky and held onto her frog pillow while watching the ceiling tiles.
They used imaging liquid to check her nissen fundoplication. We wanted to make sure that the wrap was still intact. The good news: everything looked alright.
We are still scheduled for a swallow study this Thursday at 2pm. Unfortunately, I think we still might be in the hospital. So the silver lining is that we can conveniently just wheel on down to have our tests done. The swallow study should answer a lot of our questions that we have been having about Ella’s recent retching with secretions and oral food intake. Also, it should help us come up with a strategy for increasing her calories and a better idea of what we can feed her orally over the coming days.
Once we came back, I fed Ella – – she was tired and very hungry (she had not eaten since 6:30am; we needed an empty tummy to check out her nissen). Once I fed her, she took a nap. When she woke up, she seemed like she was laboring more in her breathing. I kept watching her numbers and behavior. She was still on 1 liter of oxygen, but pretty congested and breathing through her mouth more. The pulse oximeter showed her in the low to mid 90’s, but then dipping down into the low to mid 80’s and not recovering quick. The process of dipping down into the 80s was happening more and more.
I mentioned something to the nurse. She watched, but then Ella would creep up into the 90’s, so she didn’t feel any action was necessary. That was my double-check or second opinion for the time being.
Later around 4pm, Ella began to complain to me a lot. She was clearly having a tough time breathing. She was staying in the 80s more and more. She looked dusky and was breathing labored and fast, with a heart rate around 185. She needed more oxygen and she was letting me know clinically by her complaining too: she was grunting. The flow meter in the room only went to 1 liter. I couldn’t locate the nurse. So I walked to the other side of the bed and grabbed the blow-by oxygen. Ella seemed to respond favorably and crept up into the low 90s. This was my confirmation that she did indeed need more oxygen – it was not my imagination.
At that time, a case manager came in to talk with me. I expressed my concern with her and she indicated that she would go find my nurse for me. Without going into a lot of detail, Ella down spiraled in approximately a 15 minute time frame. She ended up on 2.5 liters of oxygen and required blow-by oxygen to stabilize.
During this episode, they decided to draw labs again and ordered another chest xray. I had not even seen the initial xray, so I asked the doc to take a peek. As soon as I saw it, my gut instinct kicked in and confirmed it: Ella is once again retaining fluid. Her BUN is 14 and she has too much fluid on board; she does so much better when she is more dry.
The biggest change since we came home to Denver is that we were told she could have diluted juice and/or water orally, so she has been having a lot more fluid input over the past weeks. Although it was slow, it might have made the difference. She has always been fluid restricted in the past. This is the only change I can think of related to fluid input.
After going back and forth with the various doctors and sharing her history (this is a teaching hospital too, so you have to explain things over and over to several people), they decided to give her more diuretic. I explained how IV lasik works well for Ella and that it might help get the fluid off her more quickly. Since they did not have an IV yet, they opted to start by giving her an extra dose of Bumex (she gets it 2x per day, so they added another dose). Also, the pulmonologist opted to give her a steroid for the next 5 days to help with lung inflammation called Prednisolone. Hopefully, this will just help her regain strength.
The biggest challenge now: we need peripheral access. They tried to get an IV yesterday with three different people, including a charge nurse. None were successful. Today, they sent someone with a “good stick” that was able to draw labs and did not see anywhere to get in a peripheral IV. So they called the charge nurse in the NICU to come and try. She tried three different places and was not successful.
At this point, they want IV access since Ella’s condition has gotten worse. They do not want to be in a place where they need to administer in a critical situation and not have access.
Our nurse thinks that the only people on shift tonight that might be able to get an IV is the flight team. So we are going to check with the flight team to see if they might be available to try. Honestly, I am not sure how/where they are going to try. She has been pricked several times in various locations. Literally, I don’t know how it will work – – maybe a miracle?
The only other option is a central line, but that is more invasive and Ella doesn’t have a great past with those either. When they did that in the past, her IVC partly occluded.
While I was typing this post, the flight team came into the room. They surveyed and the RN found one spot she thought might work. Josh went outside and prayed fervently. The whole process was about 40 minutes, but they got an IV in her left foot. Praise God – – that was a miracle. Now, Ella is sporting a sexy go-go boot and we are waiting to see if the night crew wants to give her a dose of IV lasix.
Thanks for all the outpouring of support and prayers for the three of us. Please say a special prayer for Josh. He is feeling very stressed, exhausted, and emotionally raw. He is just having a really hard time watching Ella endure this latest challenge.
Yes, this is another valley in the journey, but we know He is ever-present and with us each moment in the hospital, as He is every day. Our prayer request is for a smooth evening for Ella, that the diuretics will begin to do their magic and that her oxygen requirement can be weaned in the next 24 hours.
Psalm 121
1 I lift up my eyes to the hills—
where does my help come from?
2 My help comes from the LORD,
the Maker of heaven and earth.
3 He will not let your foot slip—
he who watches over you will not slumber;
4 indeed, he who watches over Israel
will neither slumber nor sleep.
5 The LORD watches over you—
the LORD is your shade at your right hand;
6 the sun will not harm you by day,
nor the moon by night.
7 The LORD will keep you from all harm—
he will watch over your life;
8 the LORD will watch over your coming and going
both now and forevermore.

|
|
|
|
| |
|
|
|
|
|
|
|

UPDATE – 8:00AM (MST) (by Josh):
Tina called Dr. Perry this morning (Ella’s pediatrician) because she had another rough night. Due to her continued fever, high heart rate, and overall behavior, he recommended that she take her to the ER to have her checked out. Hopefully some tests will give us more insight into what’s affecting our girl. It could be something as simple as a cold, or maybe something else. I’ll update once I know more.
While riding on light rail, listening to Charles Stanley this morning, God put this thought on my heart. Do the circumstances around us make God any less trustworthy? In ALL circumstances, we can fully trust in Him. Praise God!
UPDATE – 11:30AM (MST) (by Josh):
Tina just let me know that Ella’s being admitted to the hospital so they can watch her overnight. Not a ton of info yet, just doing all the tests…xray, echo, labs, etc in the ER before they move her to a room upstairs. One doctor said the chest x-ray looks hazy… and that maybe her lungs are wet, but they look ok otherwise…no collapsing or signs of aspiration. We’re waiting to see what Dr. Abman (her pulmonologist) thinks. White blood cell count looks ok, so it doesn’t look like infection. She’s also not running a fever right now. She’s currently on 700mls of O2 and saturating about 95%. Heart rate is around 150. We’ve also noticed that her urine output has decreased over the last day or so.
At this time we think it may just be the fluid issue Ella has always battled, but we’ll see.
Praying and trusting.
UPDATE – 11:00PM (MST) (by Tina):
Once all the tests were done this morning, we were stuck in the ER until 4:30pm. The Children’s Hospital had every bed filled to capacity, so we were waiting for someone to be discharged. They wanted to admit Ella to the hospital so that they could run more tests and monitor her overnight.
They moved us to the eighth floor. It is a private room complete with a flat screen TV, pull out bed, bathroom and view of the city and mountains. Along with the beautiful facility, all the employees have been amazing. We have never been to a Children’s Hospital and it makes such a HUGE difference when everyone is trained to take care of children. If we have to be in the hospital, we are glad to be here. It makes the experience not so bad.
This evening, Ella has stabilized on 1 liter of oxygen. Along with her fever that returned tonight, her heart rate is around 185, breaths per minute 85-100, and saturating 93-95. So far, all her tests are not pointing to anything obvious. Her white blood cell count was normal. Blood labs came back with everything in normal range, although her blood urea nitrogen (BUN) came back at 14. If you remember, a higher number means that she is more dry and Dr. Kays liked to see it 20 or higher. The last BUN was 18, when we first returned to Denver. So she is definitely more “wet”, even though she is still on a lot of diuretics.
They took a blood gas this evening and said that it was pretty good – – they expected it to be worse, but it seems her body is compensating. For all the medically minded people out there, here were the results:
PH – venous gas 7.45
PCO2 – Venous 47
PO2 – Venous 54
HCO3 – Venous 32
Total CO2 – Venous 33
Base Excess – Venous 7.0
O2 Saturation – Venous 87.3
The chest xray came back looking slightly hazy, but not real bad. It is tough for them to comment because they have no other chest xrays to compare. Her echocardiogram shows no pulmonary hypertension; this means her medicine is working and the altitude is not causing too much of an issue. The swab for viruses (they swipe boogies from her nose) came back negative. So far, no bacteria growth for the other blood tests.
Dr. Perry called and we discussed everything that happened today. He is such a great doctor – so nice. Tomorrow, Dr. Perry will be attending on rounds so we will get to see him in person. We are going to try and have some tests completed tomorrow through gastroenterology – – we want to figure out why she is retching so much and if that has played a role in her lungs getting too wet (could she be micro-aspirating)?
We expect to be here throughout tomorrow and possibly for another evening, depending on how Ella does throughout the night. Once we meet with all the doctors and they discuss the results of all the tests tomorrow morning, we will have a better idea.
Thanks for all the thoughts and prayers for the Bun. The support out there from all of you is so encouraging during times like these.

|
|
|
|
| |
|
|
|
|
|
|
|

Ella has not been herself the past 24-48 hours. Along with the increased coughing and retching, you can just tell that she doesn’t feel that great. The smile above was one of the rare glimpses throughout the day.
She felt warm, so we gave her Tylenol a few times today. Dr. Perry told us to expect that Ella might have a fever for 24-48 hours due to the vaccines. If Ella doesn’t seem improved by the morning, we will be calling Dr. Perry. These symptoms started last Friday night, but seem to be sticking around.
Her retching was so bad this morning that she passed out briefly. She has done this a few times to me over the past few weeks. But Josh was taking care of Ella this morning when it happened. It freaked him out a bit. I don’t think he has ever seen Ella get that bad with retching.
It all seems related to secretions and congestion. And today both of those things are worse. Who knows, maybe she has a bit of a cold or something. She has been breathing through her mouth more, since her nose seems to be more congested, and she seems to be requiring more oxygen.
Even at night while asleep, she is requiring more oxygen and her heart rate continues to be higher than it should be – – higher than her baseline.
When you can’t get Ella to break much of a smile, even with coaxing and funny faces, you know that she isn’t feeling well. Typically, these symptoms do not point to a good direction for Ella.
Please pray that the Bun will begin to feel better.


|
|
|
|
| |
|
|
|
Posted ( jooosh) in All Posts on August-2-2008 |
|
|

We had a bit of an early morning scare with Ella today. Something woke me up around 2:30am this morning, and I decided to go check on Ella. Her heart rate was fluctuating between 145 and 155 bpm and she wasn’t saturating that well (upper 80’s, low 90’s). She also felt a bit warm to me.
Normally I would go wake Tina up and get her thoughts, but because I tend to overreact in these kind of situations, I decided that it wasn’t critical enough to justify waking her up. I continued to check on Ella for about an hour, and then finally fell back to sleep.
Tina went in to check on her around 6:15am and I could hear Ella in the monitor. She began to cough, and then she began retching. It sounded like she couldn’t catch her breath, and then she started getting real upset. I went into the room to see if I could help Tina.
I immediately became alarmed because her heart rate was over 200bpm! We’ve seen her do this before while she was in the hospital, but not since we’ve been home. My anxiety was compounded by the lack of sleep so what started as good intentions to help Tina, turned into Tina having to take care of another upset individual.
Of course I was thinking worse case scenario at this point, even invisioning her just having a heart attack or something. I was also feeling guilty because maybe I should have done more earlier that morning.
Well, after Tina calmed Ella down a bit, and talked me out of rushing her to the Children’s Hospital, she reminded me of something I had thought of, but had since forgotten.
Ella did have her vaccinations about a week ago, and I thought this might play a part, but previously she would spike a temp within 48 hours or so. Tina then told me that the doc said we might see this happen in a week or two. Ahhhh….maybe that is what’s going on.
I went down to the kitchen to get some Tylenol for Ella. We gave her one dose then and another a few hours later. By noon her fever had broke.
We all got out of the house today and ran some errands around town and did some repairs on our rental properties.
So my scare this morning reminded me of last year when Ella was still very sick in the NICU. Man…talk about perspective. As you can see from the picture above, it’s still a very long way from where she used to be.
Praise God we have our little girl here to love. She is such a miracle.

|
|
|
|
|
|